Clinician Burnout – Lessons from BDO’s Clinician Experience Survey for Patient Experience and Primary Care
Health Populi
OCTOBER 30, 2023
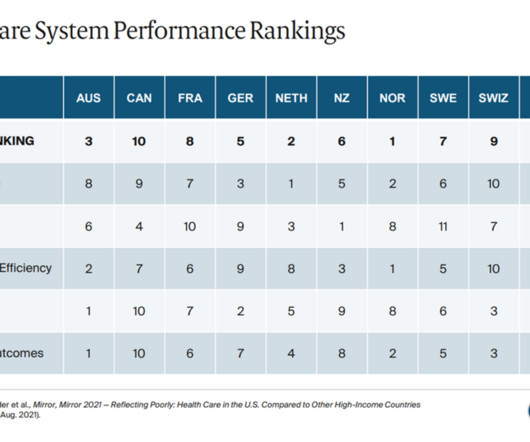
That is the profound connection between clinicians and patients that contributes to burnout and eroding morale — especially in primary care. One of the key differentiators for the high performing health systems? Strong primary care backbones for all health citizens. BDO notes that only 2 in 3 U.S.
















































Let's personalize your content