Xylazine, a powerful veterinary tranquilizer, was detected in drug tests in 34 states from every region of the country, according to a new analysis.
The analysis was conducted by national drug testing lab Millennium Health, looking at more than 160,000 de-identified urine drug test results from more than 73,000 unique patients collected between mid-April and mid-July 2023.
Xylazine, also known as “tranq,” is a sedative that prolongs and enhances the euphoric effects of illicit fentanyl. Xylazine-associated deaths are on the rise, and nearly all involve illicit fentanyl or fentanyl analogs. The Biden administration designated fentanyl combined with xylazine an emerging threat in April.
In its report, Millennium Health aimed to understand the prevalence of the drug and xylazine-associated polysubstance use in the 100 days following the emerging threat designation.
“This is a substance no human being was meant to ingest and often people may be exposed to it without their knowledge, which increases the risk," Millennium Chief Clinical Officer Angela G. Huskey, said in a press release. “This is a dangerous situation, and it’s spreading rapidly. We are trying to sound the alarm on the need to integrate clinical monitoring into our national response so we can provide advance warning and know in real-time where people need help.”
Xylazine produces serious sedation, muscle relaxation and potentially dangerous reductions in heart rate and blood pressure. Unlike opioids, it does not respond to naloxone and can cause withdrawal symptoms as well as severe skin ulcers and abscesses with repeated use due to restricted blood flow.
Prevalence differences of xylazine in East versus West
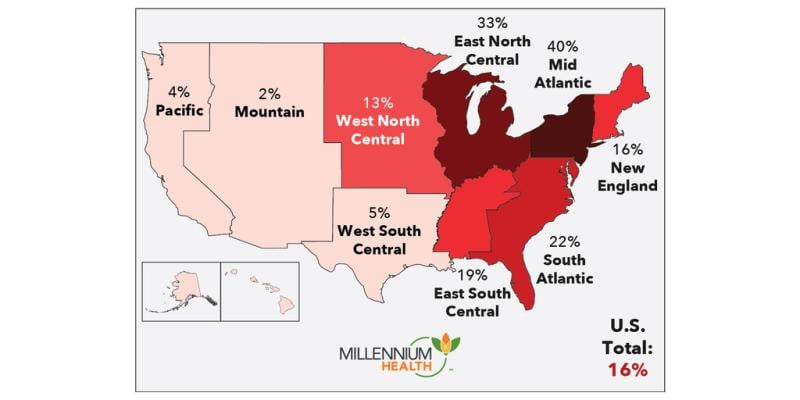
Nationally, 16% of fentanyl-positive specimens contained xylazine. But 99% of xylazine-positive specimens contained fentanyl, Millennium’s analysis revealed.
“It’s a polysubstance use crisis, centered around fentanyl,” Eric Dawson, vice president of clinical affairs at Millennium, told Fierce Healthcare.
Since the analysis only looked at drug tests ordered by a clinician, it is likely a limited view of the larger scope of the crisis. “We’re likely underreporting the true problem,” Dawson said.
The prevalence of xylazine among those who use fentanyl greatly varies by region. All regions east of the Mississippi had rates of xylazine detection in fentanyl-positive specimens above at least 13%. It was highest in the Mid-Atlantic (40%) followed by East North Central (33%). Pennsylvania, North Carolina and Ohio topped the list of states with the highest rates of xylazine detection, with Maryland not far behind.
Meanwhile, the West saw much lower rates, with the highest being in West South Central at 5%. The Pacific and Mountain divisions saw the lowest rates of xylazine use. Among those who use fentanyl in the West, California, Oregon, New Mexico and Alaska had the highest rates of xylazine use. A 2022 Drug Enforcement Administration report suggested that xylazine appears to be following the same East-to-West path as fentanyl.
Polysubstance use higher among fentanyl plus xylazine users
While polysubstance use is very common among people who use fentanyl, regardless of the presence of xylazine, polysubstance use was generally found to be significantly higher among those using fentanyl with xylazine, including drugs like prescription opioids, heroin, gabapentin, benzodiazepines, cocaine, fentanyl analogues and methamphetamine. It is unclear why, Dawson said.
More than 10% of those who used xylazine had also taken other sedating drugs, including alcohol, gabapentin and benzodiazepines, which, like xylazine, don’t respond to naloxone. The combined use with other sedating drugs is especially dangerous because their effects cannot be reversed by naloxone and can cause profound sedation that increases risk for personal injury, victimization and fatal overdose.
Provider priorities may differ, depending on their location
Clinicians in the Eastern part of the U.S. are very aware that xylazine is likely in their community, Dawson said. So providers there are focused on educating their patients about the risks and working with first responders or ER physicians to figure out the best way to manage a xylazine overdose, since it does not respond to naloxone.
There are few known drugs to help users with xylazine withdrawal. There are some early case studies being reported that involve a combination of approaches, but there does not appear to be a best practice standard at this time. “That fear of withdrawal keeps people using,” Dawson said.
Doctors out west, who may be less familiar with encountering patients on xylazine, are likely still trying to familiarize themselves with the drug and how to address it in their practice. “It’s a lot more of a fact-finding mission,” Dawson said. Hopefully, xylazine remains less prevalent there, he added.