Whether you’re a patient or a physician in the U.S., you’re burned out, tapped out, stressed out, timed out.
While the 118th U.S. Congress can’t agree on much before the 2024 summer recess, there’s one bipartisan stroke of political pens in Washington, DC, that could provide some satisfaction for both patients and doctors: bring telehealth back to patients and providers permanently.
Those pens would do two things to modernize American health care for both patients and doctors: first, Congress would pass the CONNECT for Health Act (HR 4189. S 2016) and second, re-introduce and sign the Telehealth Modernization Act. 
Why this call-to-action on the 118th U.S. Congress to address telehealth right now? Plainly put, we have 20th Century laws governing 21st century health care delivery. We have the opportunity to modernize U.S. health care, bring people back into the system, bolster physician well-being, and deliver on the promise of high-quality care that the U.S. has known how to deliver. Unless these legislative proposals are signed into law by summer 2024, the nation will have lost precious time to assure health citizens and providers alike that they can receive health care when and how they need it.
Too many patients have not returned to the health care system. Many patients in the U.S. have still not returned to usual care, some delays due to cost and some postponing needed care due to concerns about exposure to viral risks. The latest research notes that the volume of preventive screenings in the U.S. have not returned to pre-pandemic levels, which can result in later, more dire and more expensive diagnoses for patients and families, employers, communities, and the economy-at-large.
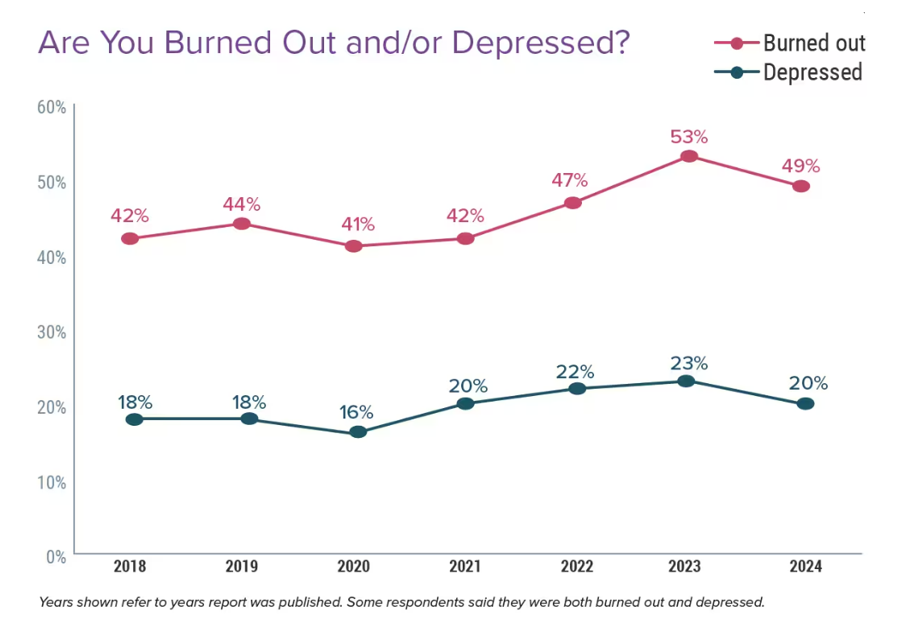
Clinicians can’t be cloned….but telehealth can help scale precious human capital. Providers are burned out, in clinical shortage situations, and many contemplating retiring earlier than planned. Deploying telehealth with assured payment regardless of communications format would help practices better manage schedules and professional resources allowing licensed clinicians to each practice at the top of their license, conserving in-person “facetime” for those patients requiring in-person encounters.
Consulting cross-borders: a bridge (or border) too far? Clinicians continue to be concerned about licensure required which has historically preventing doctors from consulting with patients residing in states in which the doctors are not licensed to practice. A physician practicing and licensed in Ohio recently shared a scenario with us about a patient he had been treating under the pandemic health emergency era living in West Virginia. To protect his licensure, the doctor asked the patient to drive from his home in West Virginia across the border into Ohio and “pull into a McDonald’s parking lot” from which the patient could access Wi-Fi and engage with the Ohio-based doctor for the consultation. This, to assure the physician that he would not be tracked by the sort of FBI state licensing compact concerns described in the linked article above.
Mental health can be scaled with telehealth. The U.S. map and citizens’ access has been marked with mental health supply shortages. The pandemic era relaxation of state licensure requirements addressed this chasm, providing greater access to patients who needed services as well as de-tabooing that access when patients felt nervous about in-person visits to therapists in a community, in-person setting. Mental health via virtual platforms has sustained significant use since the waning of the public health crisis. But pent-up demand remains for mental health services which could be made further accessible.
Younger people are more likely to demand and be comfortable with virtual care platforms. The increase of deaths and impact on lowered life-span in America was named Deaths of Despair by Sir Angus Deaton and Anne Case, Princeton researchers who tracked the dramatic uptick in U.S. deaths due to accidents, accidental overdoses, and suicide in 2017. In 2024, deaths of despair are skewing younger in what Larry Summers has termed the deepening life expectancy crisis: juvenile death. It is a critical time for the U.S. to expand access to integrated primary and behavioral health care to younger people in America, and telehealth can be a practical and even desirable platform for doing so particular for the nation’s younger patient population.
Health care happens everywhere. In fact, most people living and working in the U.S. are living omnichannel lives: whether in retail via ecommerce, buying online and picking up in store, or banking online, or studying for college degrees via Coursera, people live, work, play, pray, and learn offline and on-, in real-time and asynchronously. Health care is undergoing similar digital and omnichannel transformation following other industries.
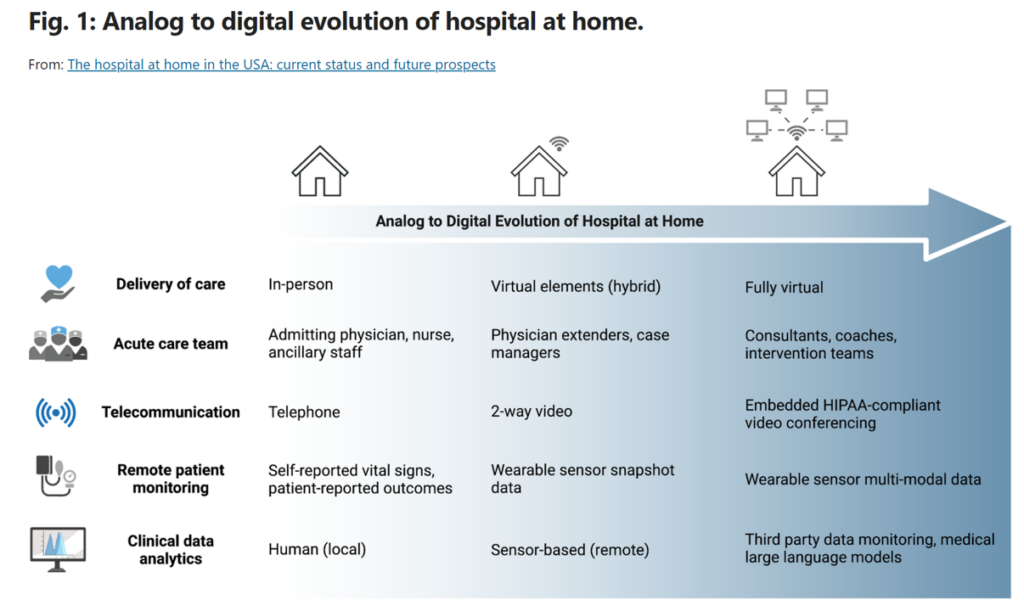
Hospital care is coming home. Most patients given the choice would rather receive acute, hospital-level care in the comfort, safety, and hygiene of their own homes. The shift of inpatient care to what’s known as Hospital-to-Home (or “at-Home”) emerged before the pandemic emergency, during which the government provided incentives for providers to participate in this clinical innovation. There is now momentum building for care coming home, with the need to keep incentives in place and, for the benefit of both patients and providers as well as cost-savings, build on the previous program.
Paying for value across the omnichannel. This digital transformation speaks to the importance of paying for health care regardless of whether services happen between patient and provider face-to-face in real-time, via video calls on-screens, or during an audio-only telehealth visit (a clinical phone call). Under the Consolidated Appropriations Act 2023, extensions for telehealth flexibilities were assured through December 31, 2024 to include audio-only telephone evaluation and management services. As of now, after December 31, only mental health services would be covered for audio-only.
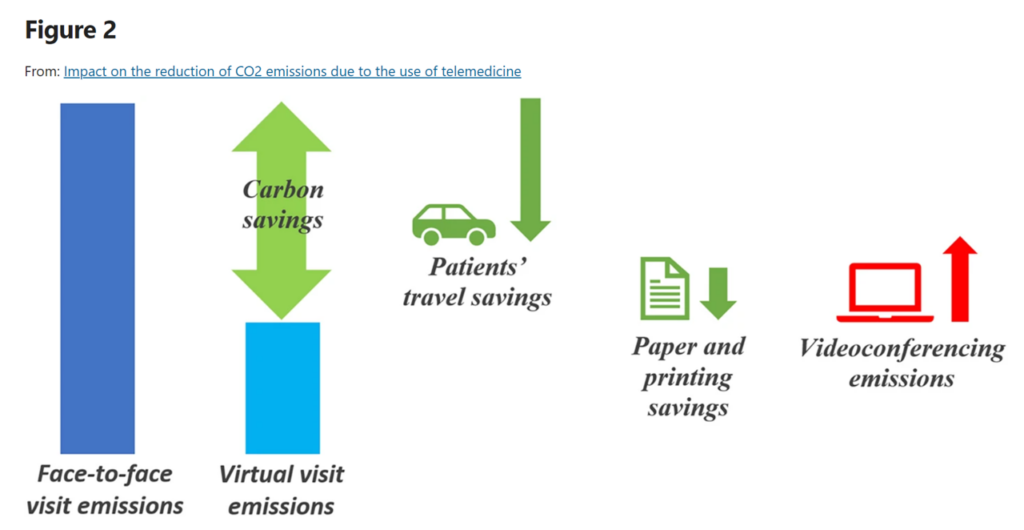
Convenience isn’t just a nice-to-have: it has economic ROI. Patients-as-consumers increasingly expect retail-enchanting service levels from health care – especially as patients pay medical bills increasingly out-of-pocket. Convenience can take the form of time: for example, time to drive to an appointment and/or time required to be away from work to attend to that appointment. A patient’s job and wages can make it difficult or impossible to take that time away from the workplace during typical physician office hours. Transportation, too, has implications for carbon footprint production, with telehealth having the potential to reduce emissions.
A call-to-action: it’s an “and,” not an “or.” Telehealth extends to health citizens living in every U.S. state, from rural communities to urban cores, not red or blue, but inclusive of every shade of patient and clinician. The 118th U.S. Congress has the opportunity – the obligation – to modernize U.S. health care the public’s health with a vote before the Congressional summer recess to make the pandemic health emergency’s telehealth provisions permanent.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.