Clinicians’ feeling burnout is the top morale challenge facing U.S. doctors, driven by turnover and understaffing, compassion fatigue, and challenges using digital tools — think EHRs. The 2023 BDO Clinician Experience Survey “takes on” clinician burnout, connecting the strategic dots between the clinician experience and the patient experience.
BDO surveyed 153 clinician leaders in June and July 2023; one-half of the clinicians were executive leaders, and one-fourth were each direct clinician providers and clinician directors. Roles reached into the C-suite (one-third), and other levels in their organizations.
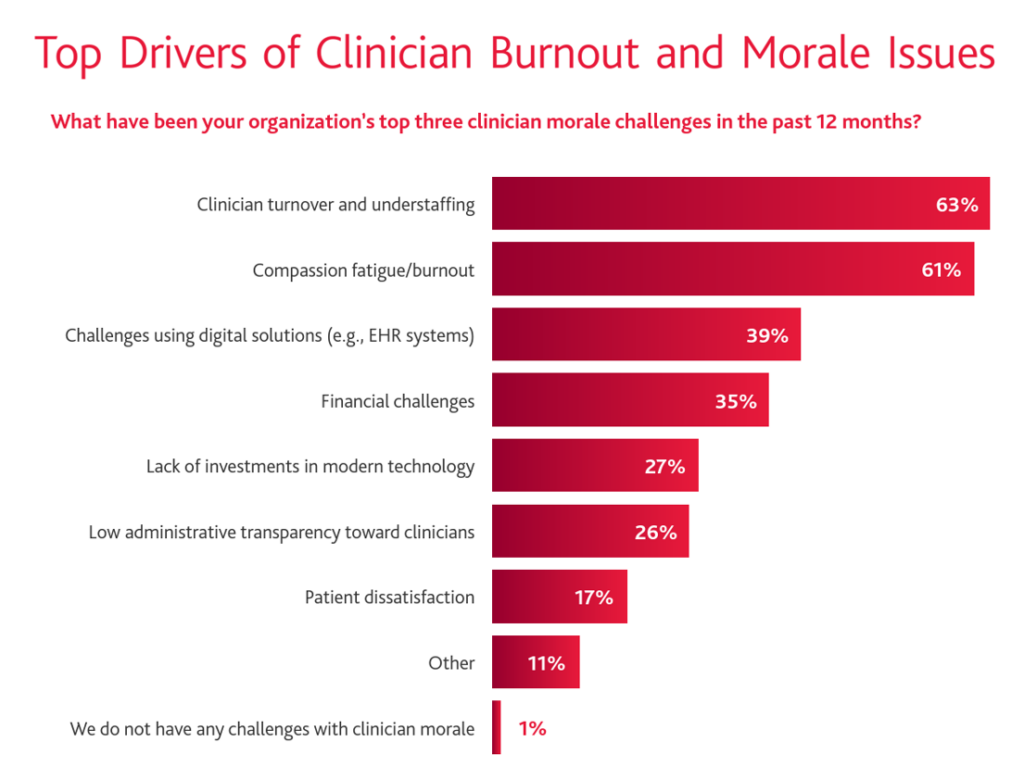
Two main factors underpin clinicians’ feelings of burnout: turnover and understaffing, and compassion fatigue, shown in the graph among two-thirds of the providers in the study. Morale was also compromised by digital technology challenges, as well as financial challenges.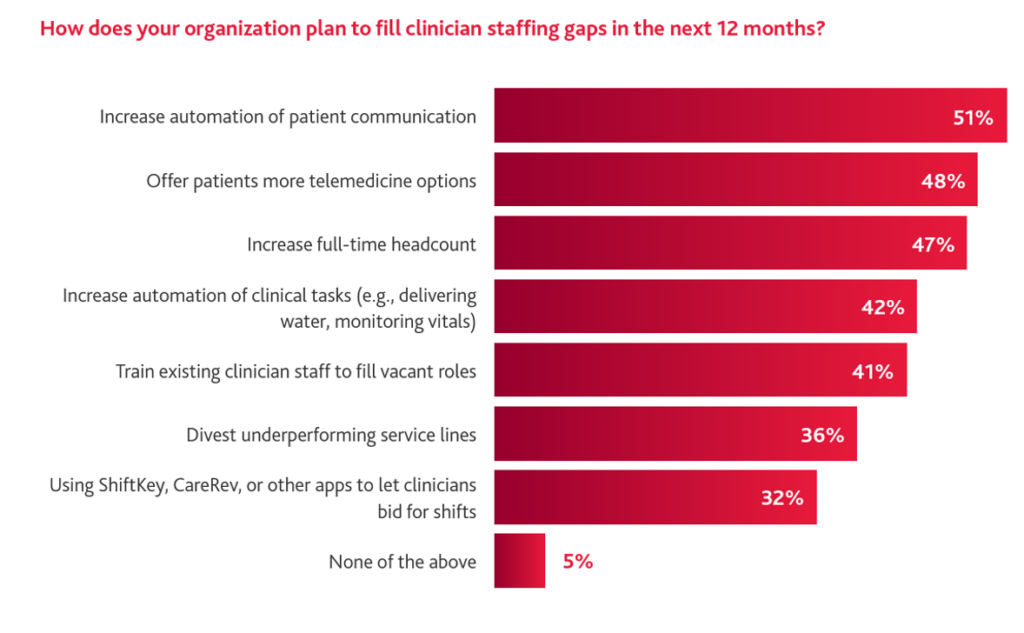
What do these clinicians’ organizations plan to do to fill in the staffing gaps that drive burnout?
About one-half of clinicians’ enterprises are looking to increase automation for patient communication, expand telehealth options to patients, and grow full-time headcount.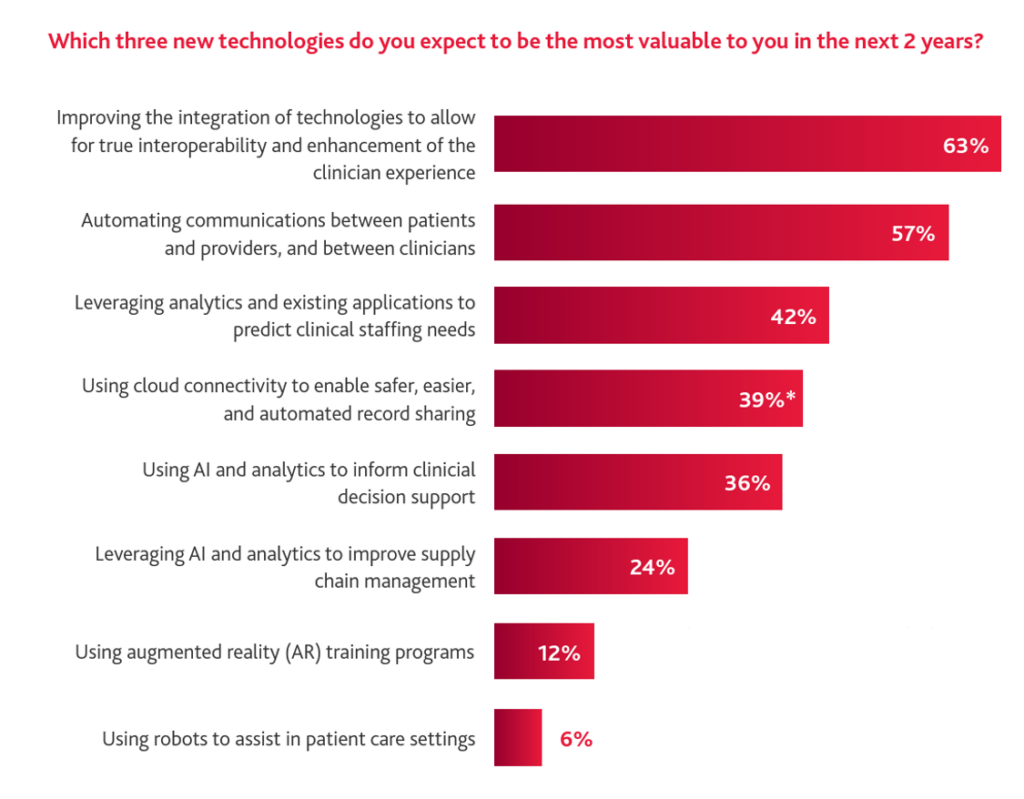
“Demanding workloads, compounded by increasing administrative responsibilities, are creating industry-wide burnout, which is only worsened by pre-existing staffing shortages. The resulting chronic turnout leads to increasing turnover, creating a cycle that can permanently damage providers, clinicians, and patients,” the BDO report notes.
Thus is the connection between physician/clinician experience and patient experience — which can be helped through adopting the right technologies and programs that directly address the root causes of burnout.
Implementing systems that improve effectiveness and efficiency are the top draw here among clinicians, followed by meeting with the doctors to gain an understand of their needs.
And third, investing in clinician mental health resources garnered 42% of clinicians’ interest in the BDO survey.
Getting to interoperability of systems and data is key, and BDO provides a helpful sidebar int he report speaking to getting more of your EHR system. Optimal use of EHRs can help lower administrative costs and better focus on workflows.
How to move forward? BDO asks and answers. BDO identified three strategies:
- Expand virtual care options, perhaps automated chatbots that can deal with minor and non-urgent complaints — reducing the burden on clinicians;
- Make the most of current staff, enabling clinicians to work at the top of their license; and,
- Prioritize key services, by service lines and/or specialties — ensuring, too, that critical services continue to be offered in the organization’s local target community,
Health Populi’s Hot Points: “Digital patient engagement tools have become essential for patient acquisition and retention. Additionally, these tools support more efficient practice operations, which have become critically important as practices face labor challenges,” Brad Boyd, BDO’s National Co-Leader in the firm’s Center for Healthcare Excellence & Innovation, observes in the study report.
That is the profound connection between clinicians and patients that contributes to burnout and eroding morale — especially in primary care.
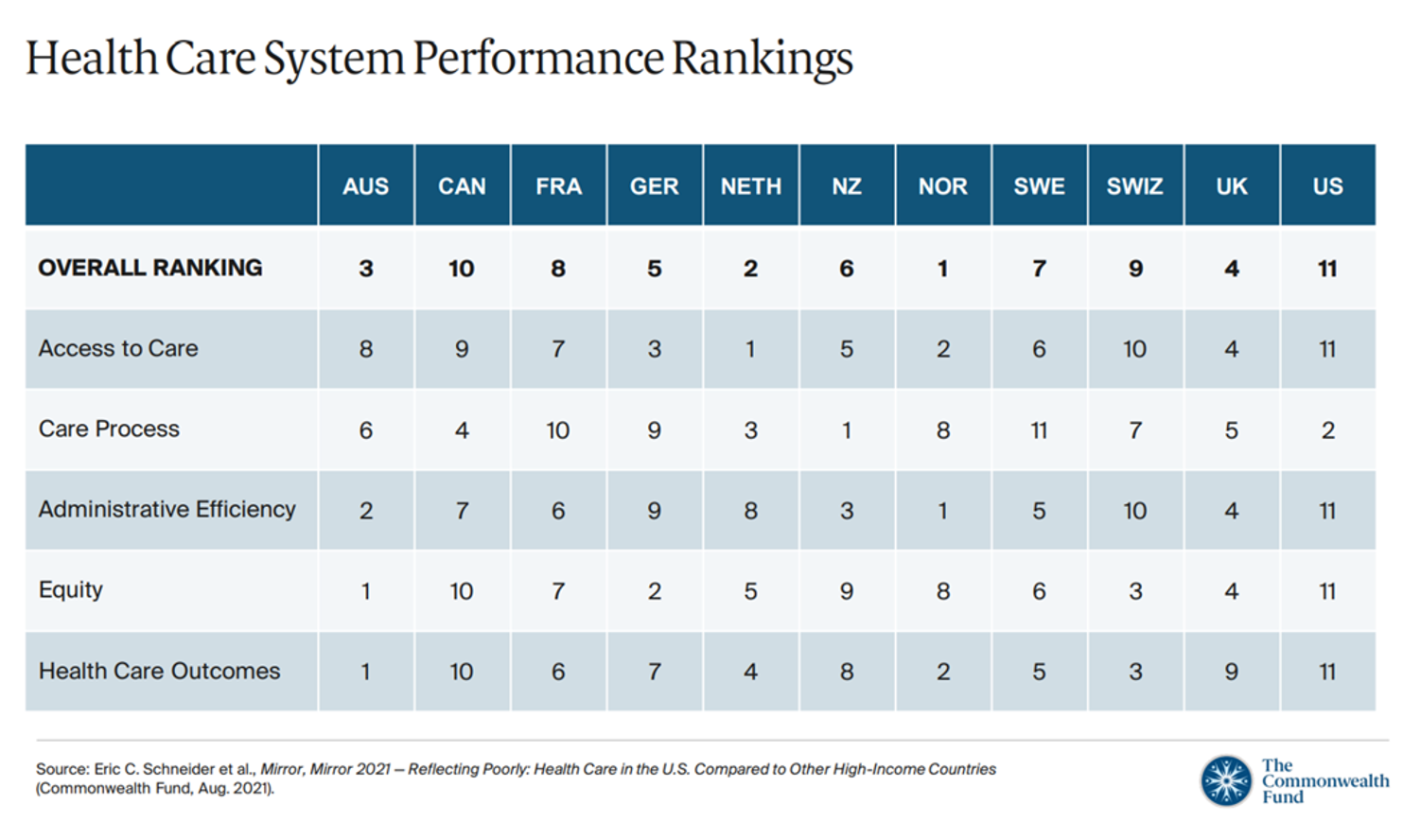
Primary care is the backbone of every high-performing health care system in the world, we have learned over the many years The Commonwealth Fund has conducted research into high performing health systems. Measures of high performance include affordability, equity, and avoidable deaths, among other metrics.
“Many countries achieve better outcomes despite lower spending,” the Fund asserts, citing Australia, Norway, and Switzerland with lower infant mortality rates and high life expectancies. One of the key differentiators for the high performing health systems? Strong primary care backbones for all health citizens.
BDO notes that only 2 in 3 U.S. patients had regular sources of primary care in 2023.
In the current U.S. health/care ecosystem, we are seeing growing retail health formats for primary care in what I’ve coined as the primary care battle royale. More patients are keen to access care at home and closer to home in their local communities, far from Pill Hill or the Medical Office Building with costly parking garages.
Do these newer models of primary care further fragment care and add costs or improve access and outcomes? It’s too early to tell. But one key success factor to make this work for both physicians and patients is to ensure that providers invest in and implement enchantingly-designed information platforms and health data ecosystems that capture patients’ data and allow for both patient and provider to access the health information they want when and how they need or want to.
We’ll keep our eyes on ongoing developments for such health data ecosystems and platforms, tracking how each side of the patient-doctor relationship can be buoyed — and not burned out — by these IT systems.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.