An aging U.S. population with a preference for growing older at home — and a fiscally challenging health care financing outlook — are setting the demographic and financial table for the shift of medical care to peoples’ homes discussed in The State of Health at Home Models: Key Considerations and Opportunities, published by the American Medical Association (AMA).
Note that this framework has been developed by the AMA, the largest professional organization of doctors. While moving health care to the home will involve quite different workflows and disruptions to current general medical practice, it is clear that physicians in the U.S. are coming to understand the benefits, as well as the realities, that will foster a move to more health care delivered where people live in environments that promise to be safe, comfortable, and familiar.
As the introduction explains, “delivering care in the home has emerged as not only a possible solution to points of friction, but a way to transform how we think about caring for patients.” 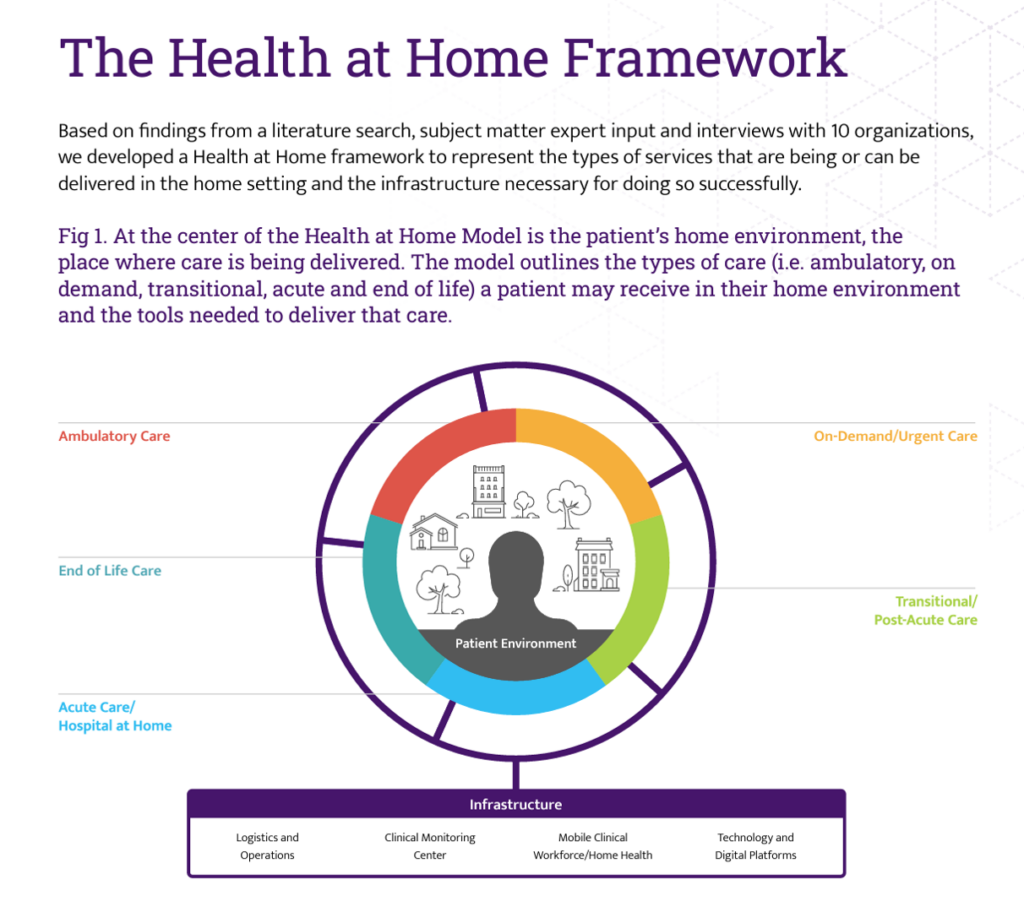
The H-a-H Framework is illustrated here, with the patient’s home environment is positioned at the center of the circle which identifies various care services including:
- Ambulatory care, covering primary care, chronic care, specialty care, mental and behavioral health, oncology-at-home, dialysis, infusion
- On-demand and urgent care, which can embed emergency medical services via telemedicine, mobile lab, at-home testing, and mobile radiology
- Acute care and the hospital-at-home flavored programs
- Transitional and post-acute care, such as home pharmacy services, skilled nursing in the home, rehab at home, and home occupational therapy, for example; and,
- End-of-life care — completing the full circle-of-life in the vision, including palliative care.
Aspects of the infrastructure for enabling H-a-H services addressing logistics and operations; clinical monitoring (think: eICU channeled to the home and remote monitoring devices communicating via Bluetooth with smart Internet of Medical Things and other IoT devices that can support peoples’ well-being at home; mobile clinical technology for the workforce (from home health staff to nurses and doctors, ancillary therapists and home infusion workers); and technology and digital platforms from Wi-Fi to HIPAA-compliant connections.
Logistics and operations addresses information processing, sharing, analyzing, and management — requiring interoperability and data liquidity, along with “nutritious” AI underpinning the analyses to ensure health equity-by-design.

As we start at this fairly nascent moment in the hospital-to-home movement and migration in the U.S., I like to plant this thought from the report into our collective thinking — wisdom shared by Dr. Anthony Wylie who is Senior Medical Director with Geisinger at Home. Referring to patient-clients, he’s observed,
“They’re welcoming you into their home, which I’ve always felt is a tremendous privilege to be able to go into someone’s home, especially when they’re ill. One of the important things that we do each and every time is acknowledge that we’re very thankful that they let us do that.”
Health Populi’s Hot Points: “Self-care is the new healthcare,” Monigle’s latest report on Humanizing Brand Experience, Volume 6, health care edition, called out.
Discussing the firm’s latest research into patient experience, the study of 3,000 U.S. consumers found that only 5% of people had received in-home healthcare in the past year, while 89% of people received care at a doctor’s office or hospital/medical facility, in-person.
In-between, though, note that,
- 42% of people engaged in self-diagnosis and self-care to manage their health, and
- 29% utilized virtual care via online video, audio and instant messaging to connect to a doctor or healthcare professional (through computer or mobile device).
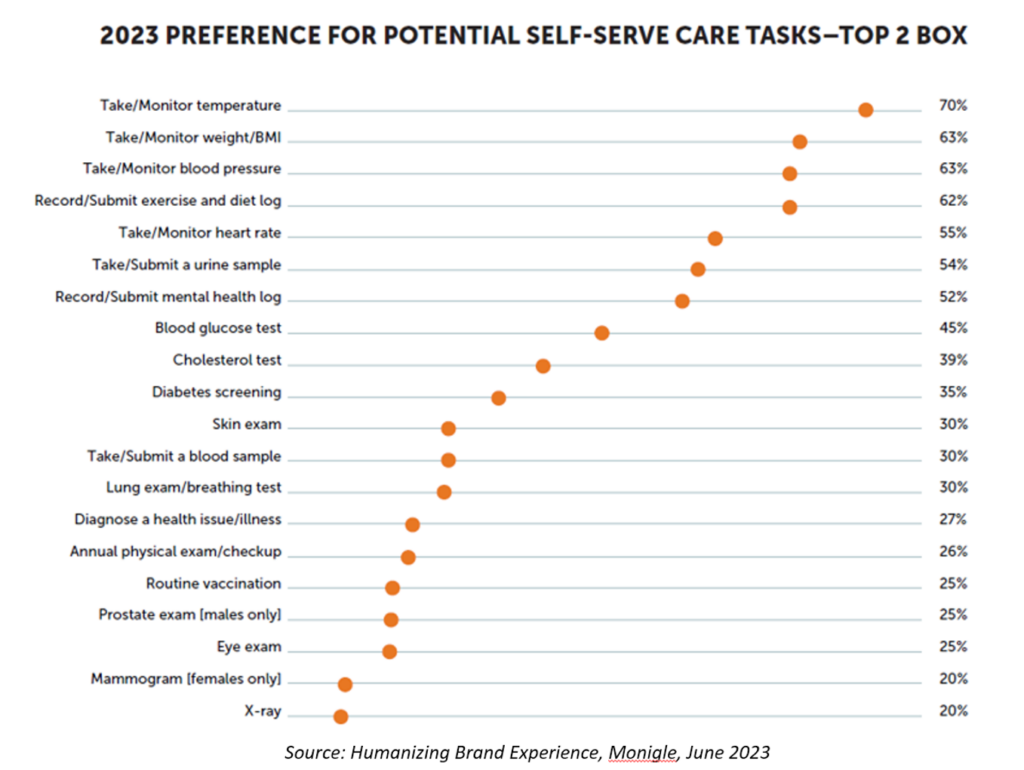
The last chart arrays tasks that consumers would be comfortable performing for self-service health care — expressing their top two preferences. More than 50% of people would take and monitor their temperature, measure their weight/BMI, monitor blood pressure, submit exercise and diet logs, monitor heart rate, submit a urine sample, and submit a mental health log.
45% of folks would do blood glucose tests at home, 39% a cholesterol test, and 35% screen for diabetes.
Increasingly, patients are adopting self-care behaviors, especially enabled through the digital devices people use as consumers — and especially mobile phones and smartwatches, favored over dedicated fitness wearables. The more health sensors on a smartwatch, the less multi-modal a consumer has to be. Consider this graphic from The Economist’s coverage of the state of Quantified Self in May 2022. Increasingly, consumer-facing devices are morphing toward clinically-excellent technologies, and hospital-based tech transforming into smaller, nimbler devices for home use and mobile workers to deploy in hospital-at-home programs.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.