There’s widespread consensus that payments to Medicare Advantage Organizations (MAOs) are a mess. These programs, which care for more than 30 million of the nearly 64 million Medicare enrollees, operate on the cutting edge of health care and suffer serious problems in data collection and billing.
A recent article of mine explored how CMS is using AI to find suspicious payments that deserve investigation. This article looks at the problem from the other side. Here, we adopt a position sympathetic to the hurdles facing Medicare Advantage plans and look at how they are trying to improve the quality of data.
A bit of cynicism is deserved here. Consultants who offer services to healthcare providers often cite “improving the quality of diagnoses” as a code phrase for “extracting the maximum payment you can for a given patient.”
I talked recently to Meleah Bridgeford, senior director of risk adjustment analytics at Episource, about how their analytics and billing solution can improve the quality of submissions and payments at Medicare Advantage plans. She says that quality has to be balanced; you need a system that honestly counts both missing diagnosis codes that can increase CMS payments (“adds”) and codes that don’t meet standards and require the plan to remit payments back to CMS (“deletes”). Figure 1 shows a typical dashboard from Episource.
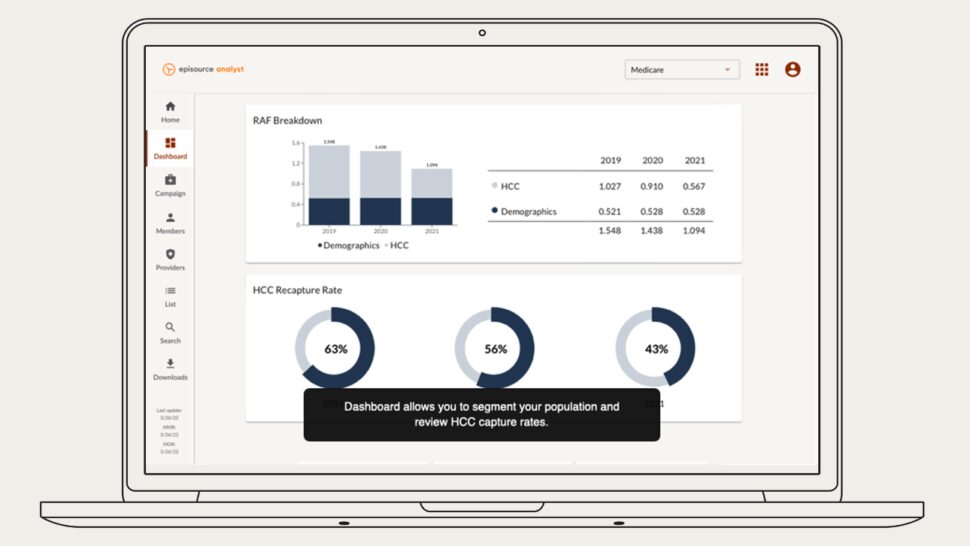
Chart reviews are independent examinations of patients’ clinical records. They’re valuable for many reasons. CMS requires chart reviews to catch overpayments. But Medicare Advantage plans do their own chart reviews to improve the quality of care as well as to avoid penalties from CMS.
Reasons for chart reviews include:
- Finding clinical interventions that weren’t correctly billed, or perhaps weren’t billed at all. If a treatment was not billed or was billed too cheaply, the plan to increase CMS’s payment. Conversely, if the treatment was improperly upcoded, the plan has to reimburse CMS.
- Directing resources most effectively. If one patient is upcoded, they may get overtreatment, siphoning money from other patients who could benefit from more resources.
- Uncovering underlying conditions that weren’t reflected in billing. Sometimes, clinicians bill only for the acute problems they treat, and don’t provide information about underlying conditions. A chart review can help Medicare Advantage add appropriate codes for underlying conditions and train physicians to code them correctly in the future.
- Highlight clinicians who need training in coding. Chart reviews can help Medicare Advantage plans evaluate the effectiveness of the clinicians they work with. Which doctors are recording visits sloppily and opening the plan to the risk of fines? The plan can work with doctors to improve reporting.
To understand how data quality affects payments as well as treatment, you have to understand that Medicare Advantage follows what is commonly known as a fee-for-value model: The plan gets a fixed payment for each patient regardless of how much the patient uses the health care system. Each patient is evaluated to determine how much risk they present. Someone with multiple chronic conditions is expected to cost the plan more than a healthy person, so CMS pays more for each payment.
Medicare Advantage programs thus have incentives to uncover and bill for every condition that introduces risk. A common example where they can let a payment slip was cited by Bridgeford: If a patient has suffered from an amputation, this condition has to be documented every year. If a plan forgets to submit a code for the old amputation in any given year, CMS treats the patient as if they have miraculously regrown the limb and won’t credit the Medicare Advantage plan for the condition.
Another subtle problem occurs if a doctor fails to report each follow-up visit by the patient. A key measure of quality used by CMS is whether the patient carries through with a follow-up visit after a hospitalization, or continues to seek treatment for a condition such as cancer. If the Medicare Advantage plan can’t prove that the patient received the mandated care, it suffers in CMS’s quality ratings and can get fined.
Thus, plans perform chart reviews every year. Episource, an end-to-end solution vendor that combines analytics, coding, and submissions, provides a lot of support for performing chart reviews and submitting the necessary deletes and adds to CMS. Machine learning identifies charts that are most likely to contain problems.
Many doctors can tell you that they don’t like Medicare Advantage plans because they make it hard to order expensive treatments and add a lot of bureaucratic overhead. Bridgeford says that a successful plan forms a positive, collaborative relationship with providers and provides them with data to improve their billing practices. Let’s hope that this ideal becomes the norm.













