
The vaccine is coming. Unless you happen to live under a rock, you’ve noticed that much of the post-election news cycle has been dominated by the back-and-forth announcements of COVID vaccine progress, first by Pfizer, then by Moderna, and finally AstraZeneca. As an aside, I definitely enjoyed Pfizer’s bump from 90% to 95% efficacy after Moderna’s announcement…yay for capitalism? I don’t think we need to spill any more ink on that topic, but I, for one, am pumped. We are well on our way back towards normalcy, right?

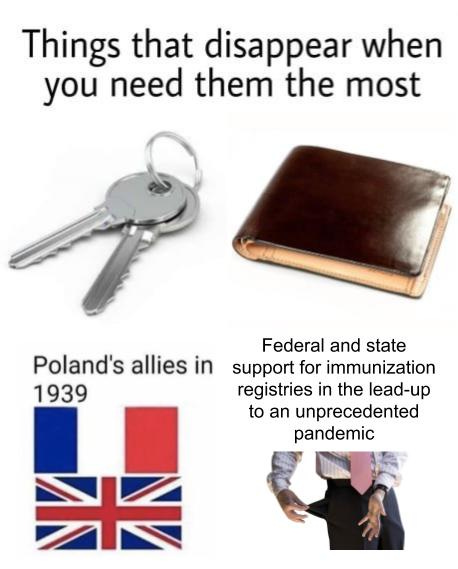
Unfortunately, despite this good news, there are still major technological and logistic hurdles between now and us all meeting up at HIMSS 2021 like “Wow, what a year that was, huh?”. And similar to literally every prior aspect of our national efforts to combat this pandemic, we appear to be woefully underestimating what’s to come.
Those challenges can be broken down into two general categories:
- How do we get it to everyone? – Production and distribution of the vaccine at a massive, international scale
- How do we ensure everyone has it? – Administration of the vaccine and associated understanding of our progress in that area
Given that the problems that I focus on most are integration in clinical workflows (and that there are many other smart minds writing about logistics – the best is Olivia’s here), I’m probably best equipped to opine on that second problem.
A typical vaccination visit typically follows this sort of outpatient encounter workflow:
- Patients are reminded of the need for immunizations by a provider at regular intervals (or decide they need one)
- The patient schedules an appointment at an outpatient clinic (pediatrician, primary care provider, pharmacy)
- Immunization is administered by a doctor/nurse (generally a shot)
- Patient, after overcoming fear of said shot, has slightly bruised spot where the shot was administered for a day, but otherwise is excited and shows off bruise to people for most of that day (what, not everyone behaves like a 12 year old?)
- Patient’s body fights off the weakened/dead agent and is now immune due to antibodies
What’s great about the upcoming inoculation effort for COVID: step 1 should be significantly easier to start. When the general motivation is “be allowed back to bars, church, sports games, and concerts”, you’ve got pretty much every demo covered. There’s a strong compelling event and heavy incentive for high average immunization compared to the random call or email reminding you about DTaP immunization.

However… with general partisanship and the change of administration, as well as some niche (but vocal) perspectives on purported vaccination side-effects, there are also stronger headwinds to full population-wide immunization.
So, from a technology standpoint, in order to get to a really safe state societally, there’s a strong need to understand (a) how immunization is going at a population level and (b) who has been vaccinated at an individual level. Functionally, this type of tool is called an immunization registry, and, luckily for us, it has existed for decades. Immunization information systems (IIS) have received special focus as part of government health initiatives (Meaningful Use 1 and 2), so every state has one or more:
(Lisa is an excellent health tech policy follow, by the way)
But unfortunately for us, ubiquity is only part of the story, as this particular function (like many public health apparatus) has withered away in recent years.
In the late 60s and 70s, despite more than a century of progress in vaccination requirements, states were still seeing periodic outbreaks of diseases preventable by immunization, such as measles. Only 20 states had laws in place requiring children to be vaccinated as a prerequisite to attending school. Even in jurisdictions with laws requiring children to be inoculated, places such as Alaska were seeing as high as 30% non-compliance. While “must-be-vaccinated to attend public school” rules paired with strict enforcement proved an effective solution, not all states had the political wherewithal to make such a heavy-handed move in the face of the anti-vaccination movement, receiving sharp criticism for removing individual choice (okay, technically true) and potentially scaring people away from ever receiving medical care again (…wait, what).
Population-based registries were the answer. By aggregating regional data, these repositories help to raise immunization levels with child-specific reminders to providers as they see patients and to parents of children behind in immunizations. Another nice benefit of this approach: it can help prevent over-immunization, which is a problem I did not realize existed but apparently affects 10-20% of children.
🚨Sidebar Alert: Vaccines are not just for children🚨
You may have noticed at this point that I keep mentioning children. Much of vaccination history and focus has been on children. Preventative health starts early, so it’s only logical to strive to stop disease in children, especially since many immunizations last a lifetime.
However, this has unfortunately caused an association for some between vaccines and young age. As crazy as it sounds, the CDC and other health organizations have literally had to do marketing in order to educate the public on this fact and the most common ongoing vaccine, for influenza, deftly avoids that with its “flu shot” branding.
The COVID pandemic is actually a bit of an outlier as an emergent, cross-generational disease that may possibly be like the flu and need recurring seasonal administration.
History
Registries began, as all (debatably) great things do, with manual interfaces. Initial immunization aggregation in the late 1990s and early 2000s was based not on electronic integration, but on paper processes. Providers would submit records of the vaccinations that they had performed, which were then recorded manually. Some advanced immunization registries utilized the web, offering basic direct-entry portals for physician recording. However, the friction of such processes limited the ubiquity and efficacy of the registries as a true tool of aggregation.
With the advent of the Electronic Health Record, friction-filled paper processes or portal workflows were not enough. Immunization administration was a key workflow within the EHR; therefore, sharing that to the registry automatically seems like a no-brainer to reduce the burden on providers.
The government thought the same. Centers for Disease Control and Prevention (CDC) dished out support to states for immunizations, more than $40 million nationwide, helping the number of total immunization registries jump tremendously between 2000 and now. Perhaps more importantly, Meaningful Use spurred adoption on the provider side, requiring that providers use certified EHRs to receive Medicare and Medicaid funds. Suddenly, EHR usage was nearly universal and the immunization documentation process was electronifying at the point of care. It also mandated the submission to state IIS through integrated mechanisms…or rather, it let providers choose between one of three public health initiatives, any of which would be fantastic to have right now to fight the pandemic:
- Submit electronic data to immunization registries/systems
- Provide electronic submission of reportable lab results to public health agencies
- Provide electronic syndromic surveillance data to public health agencies
This led to an unprecedented era of government agencies spinning up new immunization registries and going absolutely HAM on branding. For that alone, we are thankful. A brief sampling with completely subjective ranking:

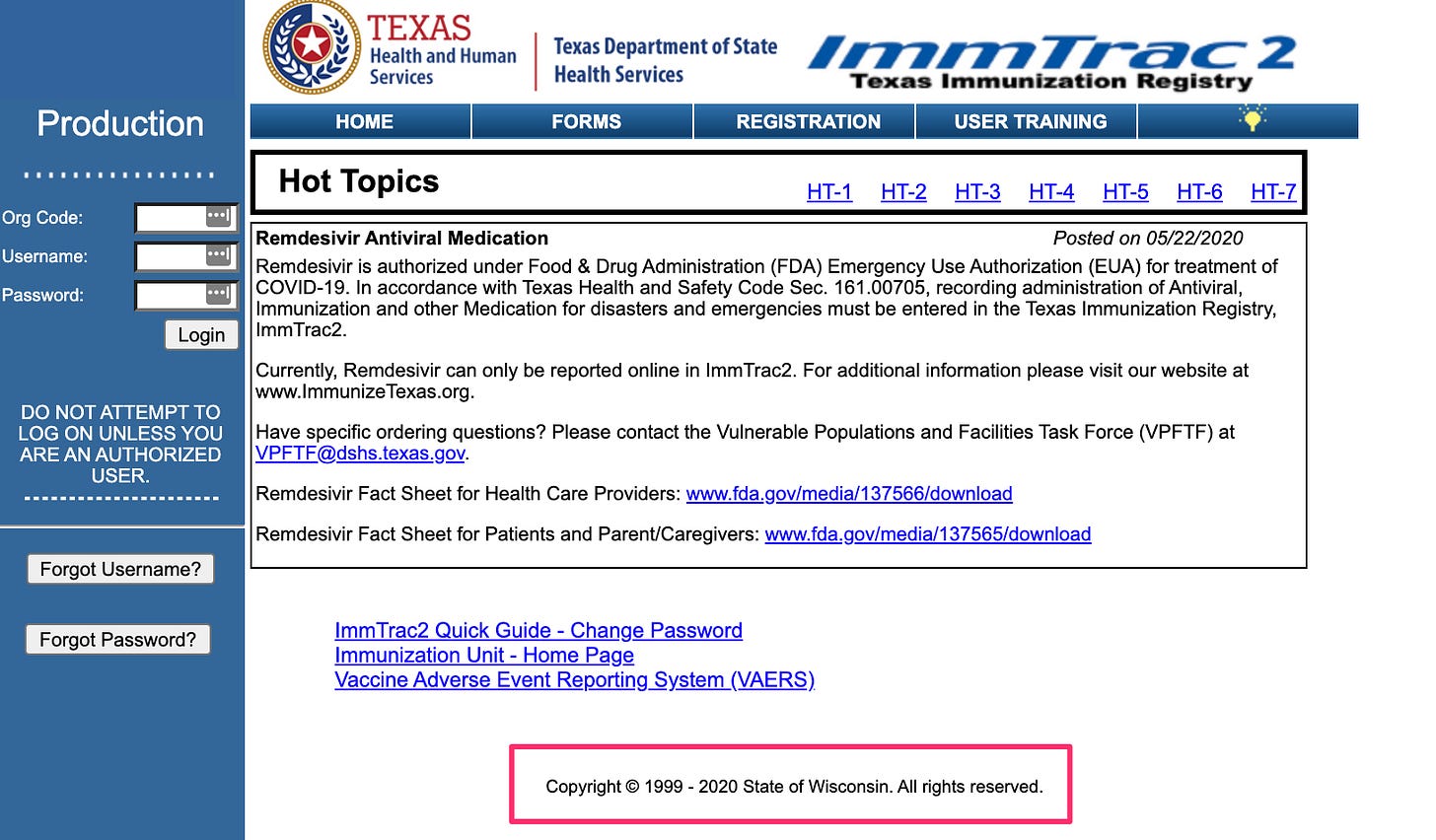



After that initial fun, the government decided to follow it up and dropped the sequel, 2̶ ̶M̶e̶a̶n̶i̶n̶g̶f̶u̶l̶ ̶2̶ ̶U̶s̶e̶f̶u̶l̶ Meaningful Use Stage 2 in 2012, and made immunization reporting mandatory unless a state had no registry. It also converged on HL7 2.5.1 as a single content standard (how the data is encoded into a format that can be decoded by a receiving party), ensuring a more uniform method across all states. However, it explicitly did not define an applicable transport standard (how the data is moved from one place to another) for the data:
ONC has made it clear that we do not require EHR technology to be certified to any transport standard, including Direct, to meet the 2014 certification criterion. Since there is no consensus transport standard that states and public health agencies use for the reporting. Therefore, ONC believes that it is appropriate for EHR technology developers to have the flexibility to include in their EHR technology and implement the transport standards that permit EPs, EHs, and CAHs to report in their states and to local public health agencies (PHAs).
This led to an acronym soup of transport methods being deployed in practice – SFTP, custom web services, MLLP with VPNs, HTTP POST with user and password in the POST body, PHIN-MS… a legacy which remains with us to this day for some registries. This breath of connectivity also left providers and their EHRs on the hook for a large surface area of supported standards.
This wasn’t necessarily negligence. In the late 2000s and early 2010s, most integration was still geared towards connecting systems within an enterprise using HL7v2 and simple transport standards (MLLP), which do not scale well to cross-enterprise scenarios. Given that there were not easily used, well-defined cross-enterprise transport standards and the fact that the government did not want to force requirements on the state agencies, they left it to providers and their EHRs to fill the gap.

Eventually, the CDC did recognize the pain here and worked with the industry to define a WSDL (a fun acronym for a transport standard’s definition) to be included in the 3rd MU installment, Stage 3 (a.k.a Return of the MU). Also included in this hot drop was a fun new feature: the ability for providers to query the registry for the historic information about a patient’s immunizations. Whereas previously doctors likely had to launch a portal, they could now view this information in the context of their normal workflows (see an example on slide 30 here). EHR vendors geared up to take on this new challenge.
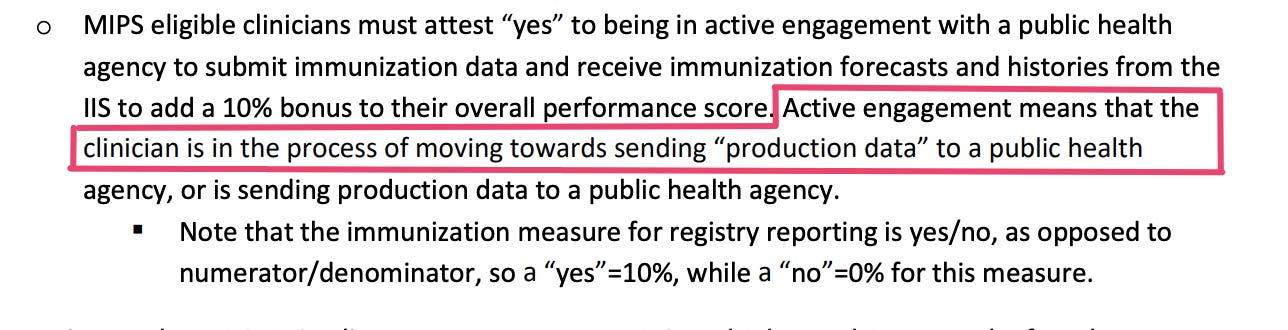
Immunization requirements still live on as Meaningful Use has turned into the Medicare Access and CHIP Reauthorization Act of 2015 and associated Merit Based Incentive Payments System (MIPS). See here the powerful language used to incentivize providers below.
So there’s been a lot of work to get these registries in place. While they were geared heavily towards pediatric purposes, they must be in shape now to help with this critical period of the pandemic, right?
Not quite.
Registries and COVID
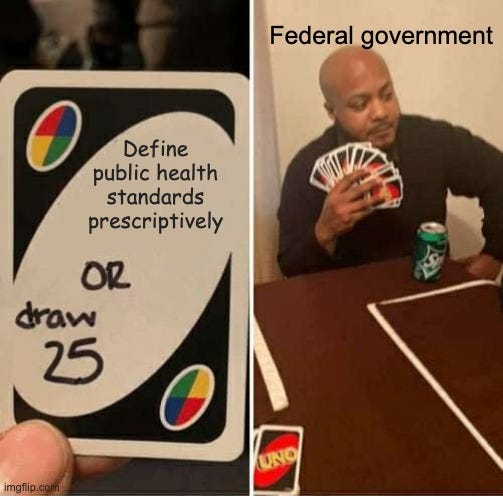
MIPS and MACRA, as well as subsequent ONC Cures regulation, haven’t been public health focused. While components of the former do call out registries, it’s only a small piece of the criteria and has a number of exceptions. Simply put, the regulatory focus for most of this decade has been on patient access, not public health. As a result, we’re missing a few key components necessary to make registries effective tools against COVID.
First, state boundaries are not hard and fast lines like national borders. We’ve seen tremendous population reorganization and redistribution during the pandemic, with commutes replaced by virtual work and mass departure from some cities such as San Francisco. Medicine is/should not be local, as the United States’ population is distinctly no longer localized. Even before the pandemic, the patterns and behaviors of this era are increasingly cross-state – traveling to college, living in a city, moving every two to four years. Decreased home buying has led to a transiency that follows opportunity clearly not constrained by state lines.
State registries do not accommodate this trend. If I go to see a provider in Oregon (where I just moved), who only can get vaccination history from Oregon, the history is… not useful. For a truly national population with a truly national problem, you unsurprisingly need a truly national solution, whether through further centralization or a stitching together of the 64 registries.
Secondly, when the COVID vaccines are rolled out to the nation, access to this history will be needed more broadly than just providers (please refer to the bouncer meme earlier). Employers may drive their return to work plans off this data. Schools may enforce it as a prerequisite as they’ve done with other immunizations. It’s even feasible that large events like concerts or weddings may hinge on immunization. Widespread access to this data is therefore needed, but without compromising privacy. Patient-driven access, therefore, becomes a tremendous part of our national picture, utilizing the patient as an intermediary for the data to ensure consent.
Luckily, this is something the federal government recognized prior to COVID. In 2018, they launched the IZ Gateway project. It’s an ambitious project to fill in the aforementioned gaps:
- Consolidated reporting for national provider organizations
- Cross jurisdictional querying for vaccination history
- Registry to registry sharing of immunization history
As we barrel towards 2021, though, this infrastructure is only just coming into place. State registries are still connecting technically and agreeing to the various data-sharing agreements that underpin the four pillars of IZ Gateway. After decades of regulatory build-up and revision of standards, it’s still a last-minute scramble for immunization registry readiness population-wide.
There are a few things that get me out of bed in the morning – connecting the health community and allowing for national data retrieval through Carequality. Making patient identity an easy, solved problem for innovative health applications. Finding interesting content, good people, and sick memes on Twitter. The chance I might see a dog when going on a run.
The work being done to help in the fight against this pandemic is some of the most exciting and rewarding I’ve been a part of. It’s been exhilarating to help partners like Curative, Helix, Georgetown University, Gauss Surgical, Ginkgo Bioworks, Phosphorus Diagnostics, and Project Beacon connect to state agencies for electronic lab reporting in this first phase of the pandemic. As we shift from testing to prevention, I’m similarly motivated by the ways we are helping and will help – enabling provider organizations, pharmacies, and other administration sites to contribute to comprehensive records; enabling schools and consumer applications to access our public infrastructure safely; helping immunization registries with the influx of participants in their ecosystems.
If you are similarly motivated, looking ahead at what’s to come, or working on the integration problems at hand, please reach out. I’d love to learn more and connect.

