With the urgent need to identify more efficient and lower-cost health care delivery models, we look to growing evidence for digital health technologies that support the Hospital at Home (HaH) model, considered in a new review article published in late February in npj Digital Medicine, The hospital at home in the USA: current status and future prospects.
Clinicians from Scripps Research and Johns Hopkins School of Medicine collaborated on this work, calling out the relatively fast adoption of HaH programs during the peak of the COVID-19 pandemic. In some parts of the world, such as Australia and Norway, “in-person at-home acute care has gained signification traction and has been offered in most hospitals for over 15 years,” the authors note. 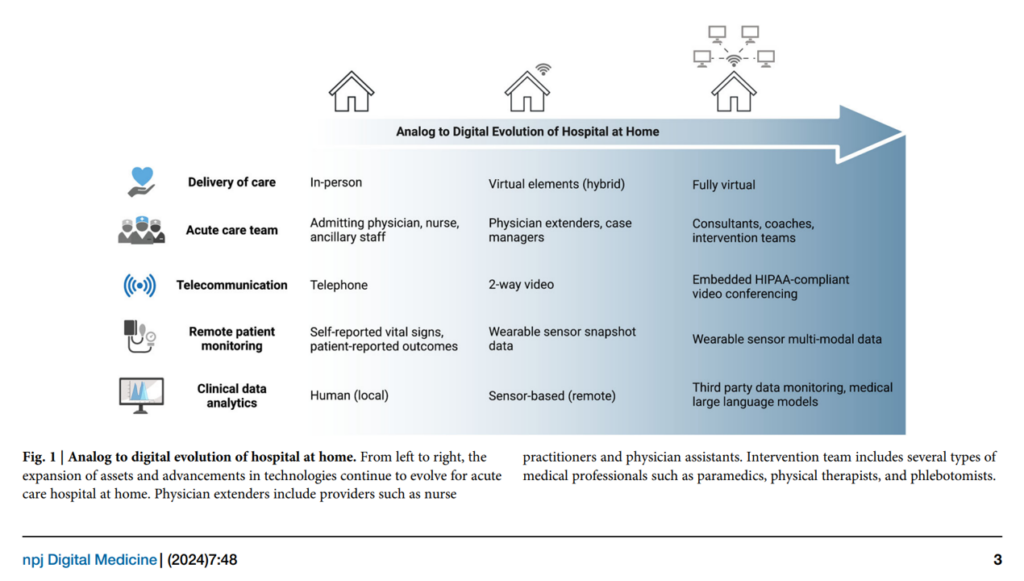
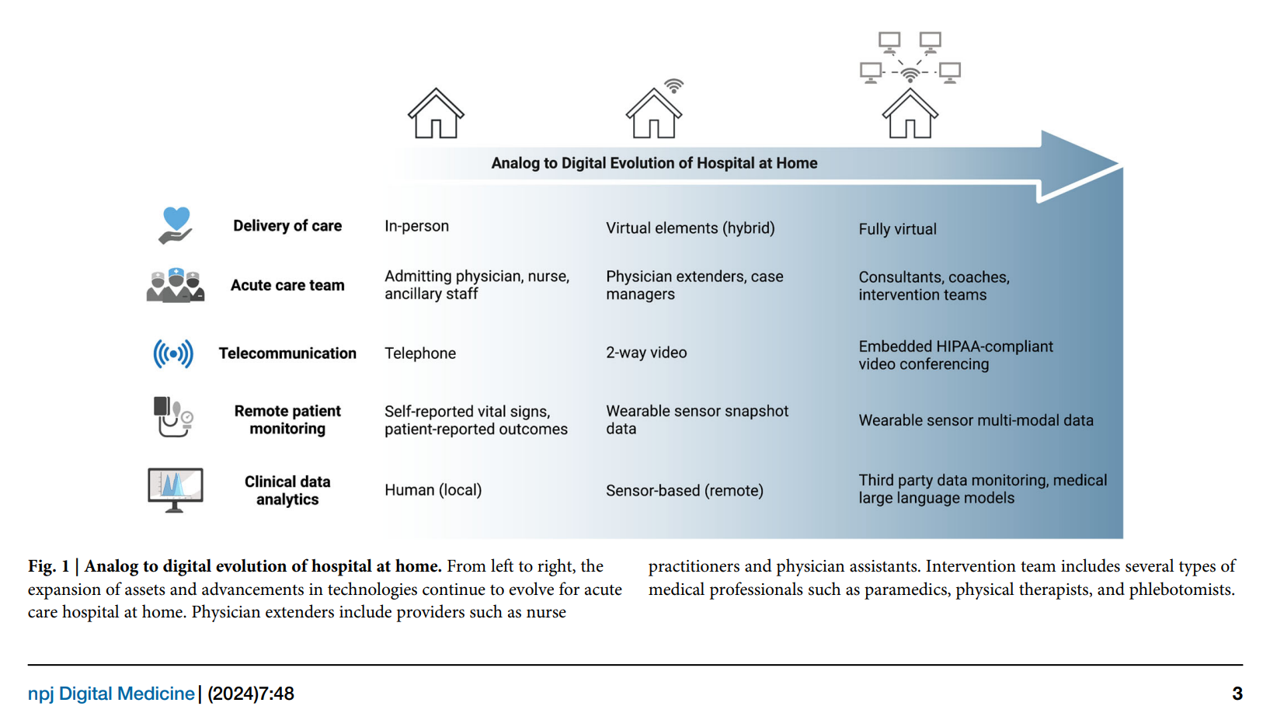
There has not been much rigorous evaluation of the “rampant” use of digital remote monitoring for acute care during the COVID-19 pandemic. The first graphic shown here illustrates the authors’ view on the digital evolution of HaH from delivery of care (migrating from in-person to fully virtual), telecomms (from telephone to embedded HIPAA-compliant video conferencing), and remote monitoring, moving from patient-reported data of vital signs to wearable sensors.
The proliferation of such wearable sensors and remote patient monitoring technologies helps set the technology stage for HaH. But a key limiting factor of these many sensors generating data has been inadequate backend algorithms that address signal noise and limited EHR integration, the authors observe.
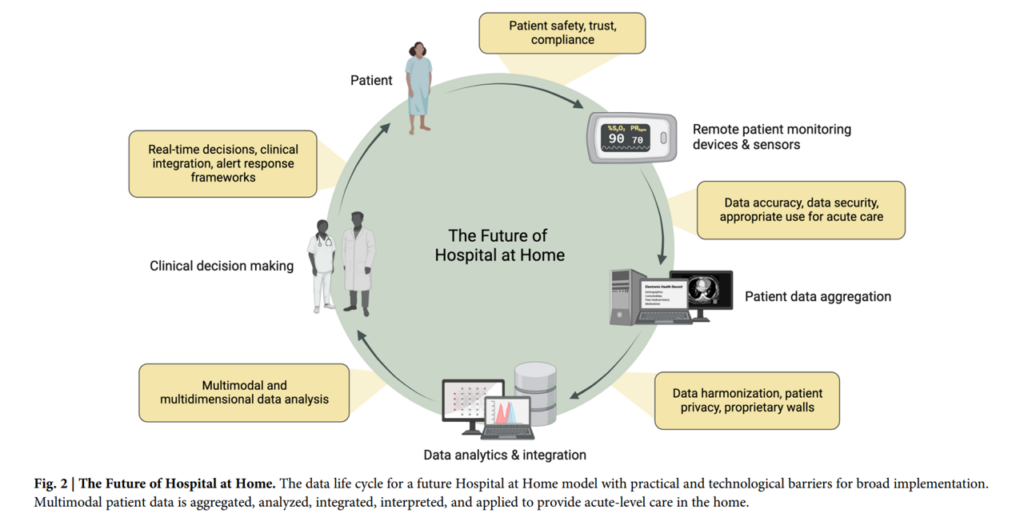
The second illustration gives us their view on the future of HaH through the lens of a data life cycle. This indicates the various barriers to implementation at different points in the patient’s HaH journey, including but not limited to:
- Analytical challenges spawned by the “ocean of possible multimodal snapshot, episodic, and continuous data” that could inform clinical insights — with the promise of large language models (LLM) and AI-based tools to support data analysis, anticipate and prevent adverse events, and bolster patient trust.
- Structural challenges, especially painful due to EHR barriers — with the promise of APIs (application programming interfaces) and the ongoing development of clinical decision support tools.
- Privacy and scalability, where assuring the security of health citizens’ protected health information (PHI) must be designed into HaH programs. Doing so is central to building trust between patients, families, and providers.
The authors also discuss the barrier of incentive conflict, with America’s volume-based “sick care” system incentivizing in-person visits and the use of services which get reimbursed. That’s a strong business model and habit that’s hard to break.
In a webinar broadcast on 28 February, Prof. Varda Shalev of Team8 discussed prospects for Care At Home Transformed tag-teaming with Deborah Di Sanzo, President of Best Buy Health.
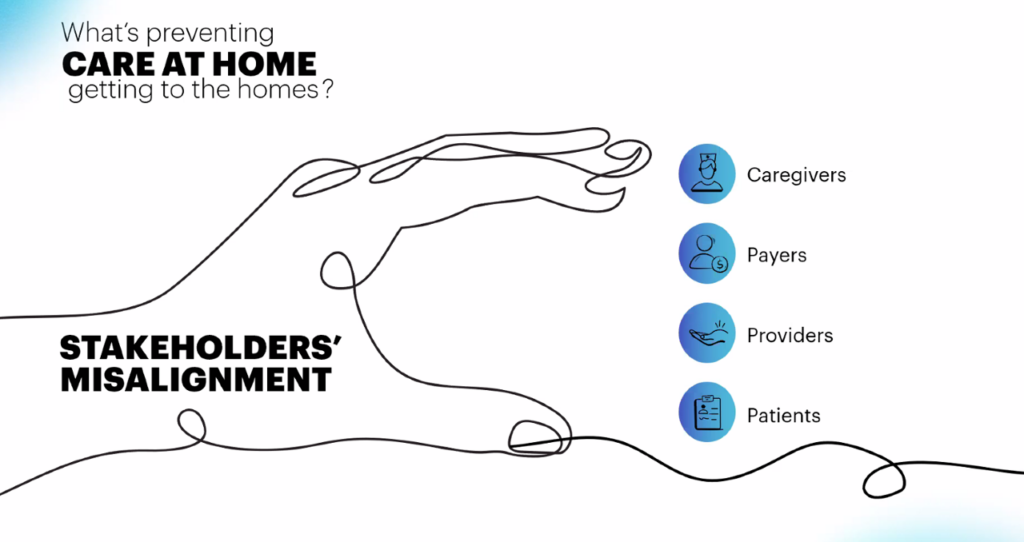
Prof. Shalev shared this diagram with us on stakeholders’ misalignment, identifying four key players in the HaH dynamic: patients, caregivers, providers, and payers. As the authors of the HaH article assert, “at a societal level, HaH could help avoid billions in capital costs to build more brick-and-mortar hospitals,” I return to Roemer’s Law learned in graduate school that, in a volume-based payment system, “A built bed is a filled bed is a billed bed.”
Thus the call for value-based payment which can, when well-designed, align the four stakeholders’ interests.
The authors of the HaH review leave us on an optimistic note in their conclusion: that “HaH models have significant promise with novel innovations” for technologies and data pipelines we successfully deployed during the pandemic era. “It is now time to rigorously evaluate their ability to become a permanent alternative form of acute care management,” they conclude in a call-to-action. 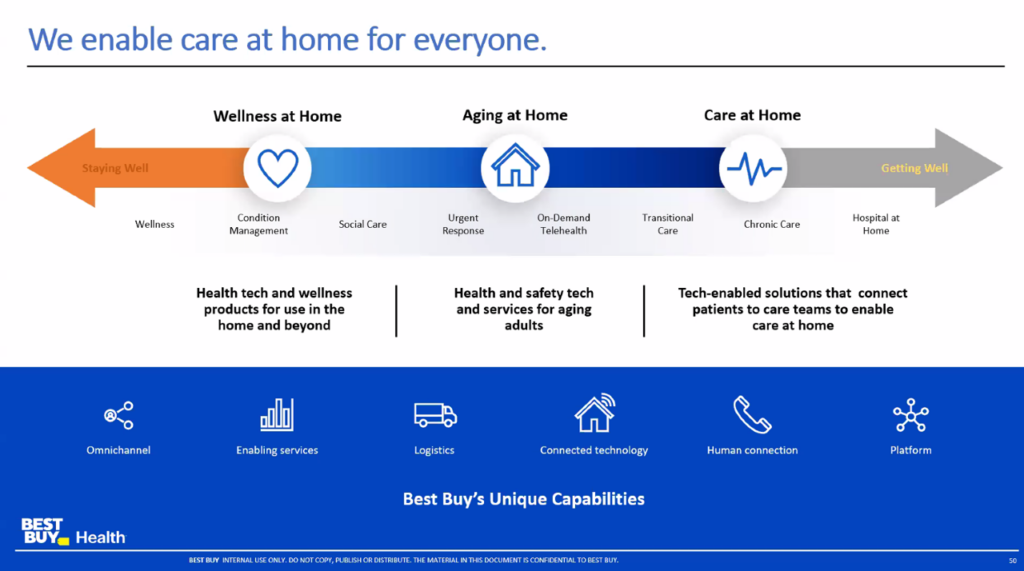
Health Populi’s Hot Points: Some of that evidence is being generated right now through the deployment of care at home channeled through Best Buy Health, which Deborah Di Sanzo discussed in the webinar. Deborah shared Best Buy’s “one-page strategy” shown here on a continuum of care from wellness at home through to aging at home and then care at home — the latter of which encompasses the HaH concept outlined in the npj Digital Medicine essay.
Best Buy Health is working with over two dozen health systems in the U.S. on care at home programs, gathering evidence and learnings across the various programs. Clearly, data interoperability and connectivity to health systems’ EHRs has been a pain point and learning opportunity for Best Buy Health, Deborah noted that even with so many data standards bodies working on this, the data coming off of the many remote monitoring and wearable devices do not all “comport” to standards — requiring a lot of engineering time to interface to all the various devices in a patient’s HaH set-up. This drives up the cost of monitoring in the current environment.
Another fascinating learning to me was hearing about the logistics required for HaH — considering that Best Buy as a major electronics retailer is masterful at logistics. Hospitals are not logisticians (with apologies to the materials management folks working hard out there in health systems). The gaps in getting various devices and technologies to patients’ homes has led to, in some cases, a Best Buy Health Geek Squad truck or van being set up in hospitals’ parking lots, which helps to address some of the logistical hiccups. 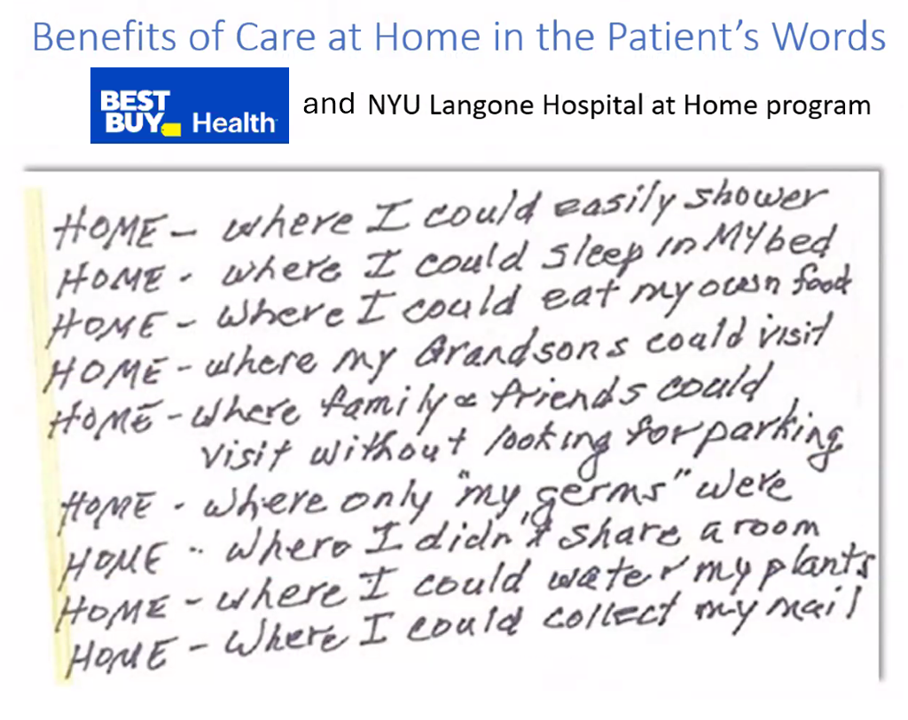
Finally, a key learning is that not all patients’ homes are ideal settings for HaH implementation. Those home gaps can deal with lack of physical space or appropriate spaces to set up the patient’s care, Wi-Fi connectivity, or lack of available caregivers to support the care 24×7 when acute care clinicians cannot physically be with the patient.
But the upside for patients embracing and loving on Care at Home are shown in this lovely slide Deborah shared with us in a patient’s own hand-writing — a patient who was part of the NYU Langone Hospital at Home program that has been partnering with Best Buy Health.
Note the value of “HOME” for health and healing, in the patient’s words: HOME,
- Where I could easily shower
- Where I could sleep in MY bed
- Where I could eat my own food
- Where my grandsons could visit
- Where family and friends could visit without looking for parking
- Where only “mt germs” were
- Where I didn’t share a room
- Where I could water my plants, and,
- Where I could collect my mail.
That’s one patient’s interests truly aligned with their HaH program.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.