https://mailchi.mp/ce4d4e40f714/the-weekly-gist-june-10-2022?e=d1e747d2d8
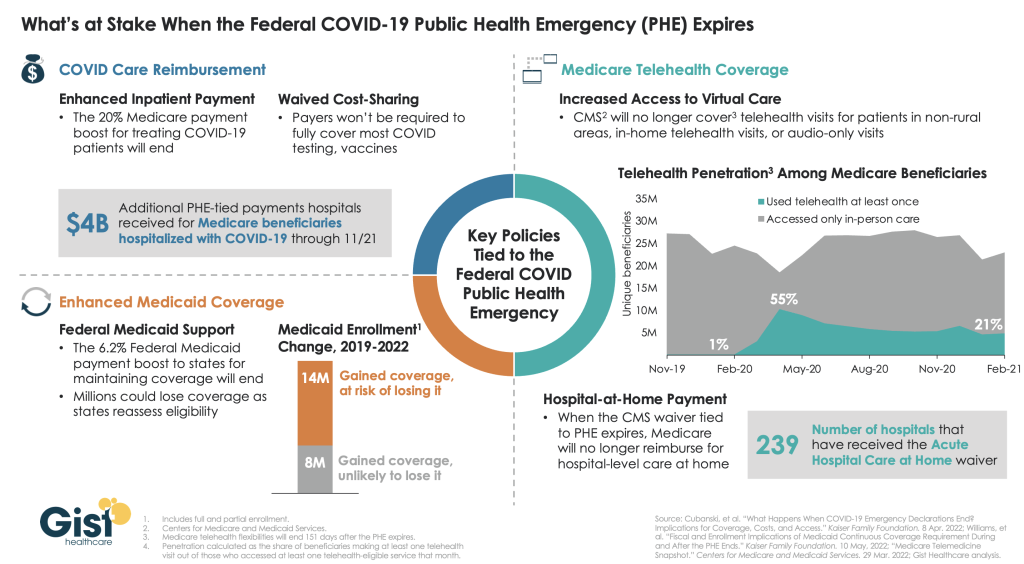
The Biden administration recently signaled that it will extend the federal COVID-19 public health emergency (PHE), which has been in place for nearly two-and-a-half years, beyond its current July 15 expiration date. As shown in the graphic above, a number of key pandemic-era policies would end if the PHE were discontinued. Hospitals, already experiencing financial challenges, would face an immediate 20 percent reduction in Medicare reimbursement for each hospitalized COVID patient.
Combined with the end of funding for treating uninsured COVID patients, and with millions of Americans expected to lose Medicaid coverage when eligibility checks restart, the cost of treating COVID patients will fall more heavily on providers. More treatment costs will also be passed on to patients, as most private insurers no longer waive cost-sharing for COVID care.
On the telemedicine front, Congress has temporarily extended some Medicare telehealth flexibilities (including current payment codes and coverage for non-rural beneficiaries) for five months after the PHE ends, while CMS studies permanent coverage options. But further Congressional action will be required to keep current Medicare telehealth coverage in place, and these decisions will surely influence private insurers’ telehealth reimbursement policies.
Although the Biden administration promises that it will provide sixty days’ notice before terminating the PHE or letting it expire, providers must prepare for the inevitable financial hit when the PHE ends.

