Three years after the beginning of the Covid-19 pandemic, there seems to be a shared feeling of disappointment on how little healthcare systems have changed globally. While structural and technological progress have indeed been slower than expected,there is no doubt the healthcare sector is experiencing a technology-driven evolution which, slowly but inexorably, will change the way we handle our health. Strong venture capital funding and increasingly frequent collaborations between governments and the private sector are just two indicators signaling a subtle but significant change. A new mindset has established : healthtech is not seen anymore as a nice-to-have “add-on” to healthcare, it is a key ally in the effort to make healthcare more accessible, agile and effective. At the same time, healthtech implementation is a prerequisite to successfully compete as a business operator in the future.
In a first article we discussed how healthtech will be key in helping us to move from modern sickcare to a healthcare approach centered around prevention and the promotion of healthy lifestyles. We also discussed how patient medical records can finally be made available seamlessly to both patients and doctors. In this second article we will discuss three more challenges impacting modern healthcare systems, showing how healthtech can improve the way : new drugs are developed , waiting lists and clinicians shortages are addressed, patients adhere to prescribed treatments.
Drug development
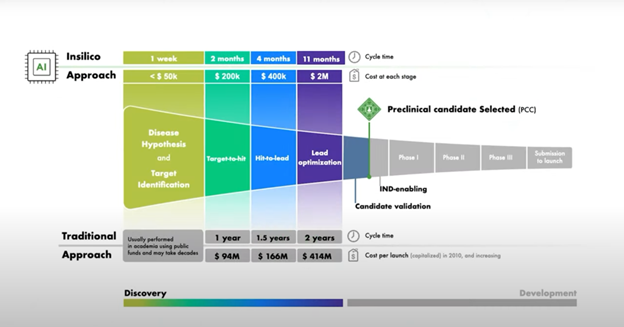
The traditional drug discovery process is characterized by its protracted timeline, high costs, and significant attrition rates among drug candidates. While average time and cost for drug development can vary widely depending on the drug, the therapeutic area, and the regulatory pathway, we can estimate that on average drug development from target identification to market approval takes between 10 to 20 years1. The cost of drug discovery and rollout can range between $2 billion to $3 billion or more2, including the costs of research and development, clinical trials, regulatory fees, and the expenses associated with drug failures. This resource-intensiveness not only hinders innovation, limiting the development of potentially life-saving drugs, but it also contributes to the elevated prices of pharmaceuticals, posing a significant barrier to healthcare accessibility for many. It is difficult to fully grasp just how much in silico medical research, driven by the fast evolution of modern generative AI algorithms, can revolutionize drug discovery and development. In biology, historically, medical trials could be carried out in vitro or in vivo: in vivo trials are conducted with a living organism, often animals, while in vitro trials take place in a controlled environment, like a petri dish or a test tube, outside of a living organism. In the 90s a new type of study was introduced in silico trials. In silico trials, which take their name from silicon-made computer chips, are trials conducted using computational models and simulation, which aim to replicate the biological processes of the human body and its organs. There are three main advantages to the use of AI in drug development: width of research, speed of execution, low costs. In the first phase of drug discovery, AI models with their computational power allow us to evaluate an extremely vast list of options when looking for a molecular target linked to a disease, potentially finding novel and unexplored correlations between molecules and diseases. Carrying out the disease hypothesis and target identification phase “in silico” empowers laboratories to find potential molecule-disease correlations without the need for expensive and prolonged academic research. In a second phase of the drug discovery process, once the most appropriate target has been prioritized, generative AI helps us design the proper molecule to tackle the target by quickly generating a set of new molecules with the needed properties. These candidates are then prioritized according to how easy they can be made, most promising ones become” lead candidates” and are sent for clinical studies. This is the methodology used by NVIDIA-backedInsilico Medicine, a leading startup in the sector. InSilico Medicine has recently entered Phase 2 clinical trials with an idiopathic pulmonary fibrosis drug candidate discovered with its AI platform. The cost and timing of Insilico Medicine’s path to preclinical candidate selection? An incredible 2.6 million US dollars and 18 months, against the standard 670 million US dollars in 4.5 years. In silico medical research cannot replace in vitro and in vivo research, which remain central in the clinical validation phases that precede approval and commercialization. However, Insilico Medicine’s numbers show that a proper use of AI can result in a very significant decrease in the financial resources and time needed to get a drug candidate to the first clinical phase.
Long waiting lists and clinicians’ shortage
Healthcare waiting lists represent a significant challenge for many countries, with millions of patients facing delays in accessing essential medical care. In England, this past July, 7.47 million people were waiting to start routine hospital treatment, the highest number since the NHS began to collect data on the issue in 20073. Long healthcare waiting time is a complex issue, closely intertwined with the shortage for healthcare workers. The clinicians’ shortage is a global healthcare crisis originated by a steep increase in the demand for healthcare services due to population growth, increase in population age and prevalence of chronic diseases. As demand grows, supply is unable to keep up because of the low capacity of training programs and medical schools or budgetary constraints preventing the employment of more healthcare workers. To this we must also factor in an issue of inefficiency of healthcare delivery, consisting in poor scheduling practices, underutilized resources, inadequate coordination of care.
When discussing healthcare waiting lists and clinicians’ shortages the public often focuses mainly on a need to increase the supply of clinicians, nurses and other allied healthcare practitioners. While this is
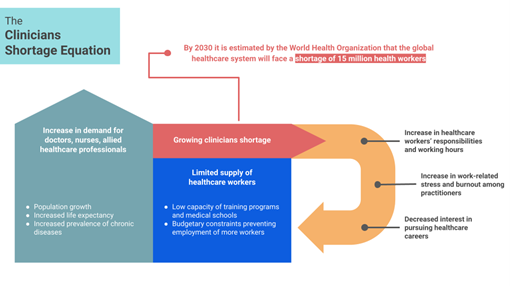
certainly part of the solution, the British NHS, which is the largest health organization in the world and the 5th largest employer globally, teaches us that simply increasing the supply of healthcare workers does not fix the issue. What allows countries like Germany, Netherlands, Denmark to have some of the best healthcare systems in terms of waiting time despite providing universal healthcare is their focus around three pillars: maximized supply of healthcare workers through proper funding of employment and training of medical workers; demand control through a focus on primary care and preventative medicine; extremely efficient administrative processes and healthcare delivery.
Healthtech can play a fundamental role in the enhancement of preventative care, as discussed previously. Furthermore, telehealth is proving to be extremely effective in maximizing the efficiency of healthcare delivery, thus optimizing the way healthcare systems respond to rising demand for healthcare services. Telehealth refers to the use of information and communication technologies for improving the conditions of the patients4, it comprises any technology enabling healthcare practitioners to either monitor and treat patients or collaborate with other practitioners while not being in the same location5. Two forms in which telehealth presents itself are teleconsultations and remote monitoring devices. Moving a significant volume of visits online, teleconsultations take weight off overwhelmed treatment facilities and minimize clinicians’ travel time, while also improving care of patients located in remote geographical areas. Teleradiology has experienced significant growth. With many European countries experiencing a lack of personnel to interpret medical images such as X-rays, MRIs, and CT scans, teleradiology broadens the pool of available radiology experts, helping countries address staffing shortages and reducing patients’ wait times. On another hand, remote monitoring devices decrease the need for recurring in-person visits thus saving time and ensuring better treatment of chronic patients. One notable success story in the realm of remote monitoring devices is the use of continuous glucose monitoring (CGM) systems for managing diabetes. In this field, with just under 2 million users and an impressive growth, Dexcom’s CGM G6 device is one of the leading solutions. By eliminating the need for frequent fingerstick tests and empowering individuals with real-time data, Dexcom’s G6 significantly reduces the need for in-person visits and facilitates remote communications between patients suffering from diabetes and their practitioners.
Patient Relationship Management (PRM) systems are also fundamental to the scaling of healthcare operations. PRM refers to IT systems implemented by hospitals or other healthcare facilities to efficiently handle the flow of information and patients. PRM systems significantly minimize waiting lines by ensuring clinicians have fast access to key medical information while facilitating real-time collaboration between doctors on clinical cases. Through PRM systems, healthcare facilities can automate communications with patients, minimizing no-shows or reallocating unwanted appointments to patients who need them. Finally, PRM systems minimize the amount of time spent by healthcare workers on administrative tasks. One example of this is the possibility to issue digital digital prescriptions and referrals, thus significantly reducing paperwork and administrative delays.
In any country afflicted by long healthcare waiting lists, underutilization of resources must be minimized at all costs. Digital appointment scheduling apps, like Teladoc and ZocDoc in the U.S. and Doctolib in Europe, give patients visibility over medical appointment slots available in their location, allowing them to book appointments or interact with practitioners through the app, thus aggregating patient demand and connecting it to healthcare supply in a more efficient way. On the other hand, American company Cohealo aims to solve the same underutilization issue, but for medical equipment. Cohealo connects hospitals allowing facilities in need of medical diagnostic equipment to request unused equipment for rent from other facilities.

Non-adherence to prescribed treatments.
Non-adherence to prescribed treatments is an issue which costs people their health, while at the same time costing healthcare systems billions of dollars yearly. Research shows that, if we look at the United States alone, every year around 125’000 deaths are due to non-adherence to treatments, with between $100 billion to $300 billion of yearly costs coming from this issue alone6. As the proportion of the population affected by chronic conditions grows, lack of adherence will soon be seen as the serious public health issue it already is. One of the most significant barriers leading to poor medication adherence is poor health literacy and, more in general, the difficulty of patients to understand the importance of drug therapy and properly follow the instructions given by their practitioner.
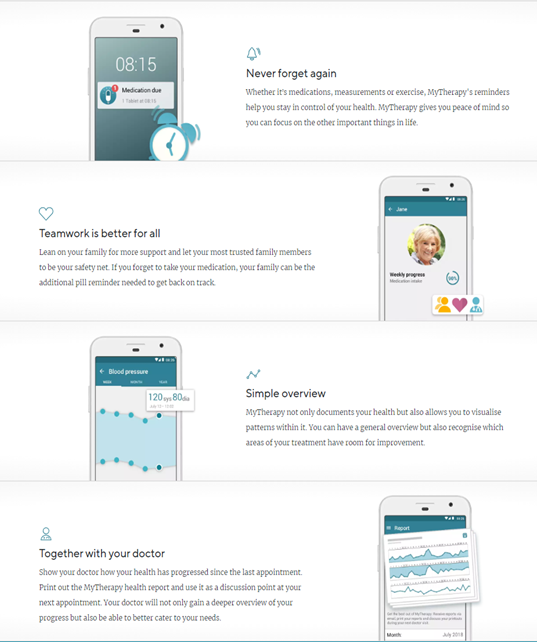
While it may be shocking to realize that patients don’t take their medications as prescribed about half the time7, it becomes easier to get behind this number once we realize how poor we are at managing the post-discharge phase of the patient journey. Today, once they leave a hospital or a clinic, most patients receive a document with a lot of information on their diagnosis and their treatment. The documents are often designed primarily for healthcare professionals, they are in fact written in medical language, which implicitly turns the patient into a passive subject. To tackle non-adherence to treatment, it is necessary to start exactly from the post-discharge phase, making the experience and tools we leave to the patients more interactive, with the purpose of effectively guiding patients through the necessary change in behavior and educating them on the importance of the prescribed drug therapy. A first solution to this issue can be found in the healthtech scope with digital patient support programs (PSPs). Patient Support Programs provide a system of homecare and online-based services to support patients, during their medical treatments. In other words, a PSP becomes sort of a virtual clinic in which patients can move freely to obtain from the specialist all the information necessary to improve their health. PSPs not only serve the purpose of educating patients and guiding them through the needed behavioral change, they are in fact a two-way tool through which the healthcare practitioner can also communicate with patients, measure the outcomes of the therapy and verify adherence. PSPs have proven to be effective in improving patient involvement in the treatment process thus maximizing adherence to prescribed treatments, minimizing hospitalizations, and containing healthcare spending. With 8 million users worldwide, MyTherapy by smartpatient is a leading PSP platform. The medication reminder and health tracking app aids patients suffering from chronic diseases in managing their treatment plans. smartpatient, responsible for developing and maintaining the MyTherapy app, partners with pharmaceutical companies and healthcare institutes, providing to patients disease-specific modules within the app. With the majority of disease-specific PSP apps produced by pharma companies failing in terms of usage and user satisfaction, smartpatient’s bet on the “operating system” model has so far proven to be successful8.
[1] “Biopharmaceutical Research & Development: The Process Behind New Medicines”, 2020, PhRMA (Pharmaceutical Research and Manufacturers of America)
[2] J.A. DiMasi, H.G. Grabowski, and R.W. Hansen, “Innovation in the Pharmaceutical Industry: New Estimates of R&D Costs”, 2016, Journal of Health Economics
[3] “NHS waiting lists hit record high in England”, 13 July 2023, BBC
[4] Roberto Ascione, “The Future of Health”, 2022
[5] Roberto Polifrone, “Sanità digitale: inizia la rivoluzione?”, 2021
[6] Regina M. Benjamin, “Medication Adherence: Helping Patients Take Their Medicines As Directed”, 2012, Public Health Reports
[7] “8 reasons patients don’t take their medications”, 22 February 2023, American Medical Association
[8] “Patient Support in MS: The Service That Nobody Uses?”, 26 July 2021, smartpatient



