Micky Tripathi, the National Coordinator for Health Information Technology at the US Department of Health and Human Services shared his interoperability wish list during his opening keynote at the 2021 Direct Trust Summit. Topping his list was richer information exchange to support advanced payment models.
I am not a tech guy, but I do enjoy learning more about interoperability and the progress the industry is making towards the nirvana of free and easy health information exchange. That is why I was excited to attend (virtually) the 2021 Direct Trust Summit.
What stood out for me was:
- The lack of worry/concern/discussion about information blocking
- Micky Tripathi’s interoperability wish list and how it reflects where the ONC is pushing the industry
- The impact interoperability can have on patient satisfaction
Information Blocking
The information blocking rule was set to be one of the dominant stories of 2020…and then COVID arrived. There were rumblings about it through the year, but healthcare obviously had other concerns. Given the lack of discussion about it at the various online conferences, I am of the belief that it’s just become part of the landscape – something that people need to comply with but not something worth raising a fuss over.
Information blocking was mentioned briefly by Tripathi during his opening keynote. “As you know the applicability date for the information blocking rule went into effect in early April,” stated Tripathi. “The ONC is now reaching out to the industry to educate everyone on what needs to be done.”
Tripathi stressed that information blocking was about more than just compliance: “We need to think about the strategic opportunities presented to your organization regardless of what type of actor you are. We need to start asking what we can do once you can get the health information that you should have access to – for authorized purposes of course.”
Wish List
Tripathi had a little fun with the #DirectTrustSummit by sharing his interoperability wish list. His list was a reflection on where the ONC is pushing the industry in terms of information exchange:
- Richer information exchange in order to support advance payment models: “Value based care is critically important and it is a key driver of interoperability. We need to move from basic information exchange to apps that will use the whole portfolio of interoperability capabilities.” According to Tripathi that includes FHIR/CDS hooks for risk assessment and shared care planning.
- Better bi-directional exchange with payers. He wants to see claims data made available to providers and clinical data made available to payers.
- Minimizing/eliminating of additional burden on providers and payers for administrative workflows. Tripathi used the example of prior authorizations – something he believes with proper and expanded use of interoperability would be much easier for healthcare staff. You could almost feel the audience nodding their heads for this wish list item.
- Doing more with electronic health information (EHI). Tripathi wants us to “get started on thinking about the kind of value that can be realized when richer health information can be more easily shared”. In particular, sharing information for faster research, better patient experiences, and improved clinical outcomes.
- Greater transparency for patients, providers and payers for prior auth tracking, claims & payment tracking, record attachments, status of referrals. “There are services levels that people have come to expect outside of healthcare,” stated Tripathi. “We need to move in that direction as much as possible.” More transparency into healthcare’s opaque processes like referrals, could make for improved patient experiences.
Interoperability + Patient Experience
Tripathi’s final wish-list item was a perfect segue for the presentation by Rakesh Mathew from HealthShare Exchange who shared a case study of a health system that implemented an app to help patients and referring physicians find a doctor.
After almost a year of using the app, the results were less than stellar:
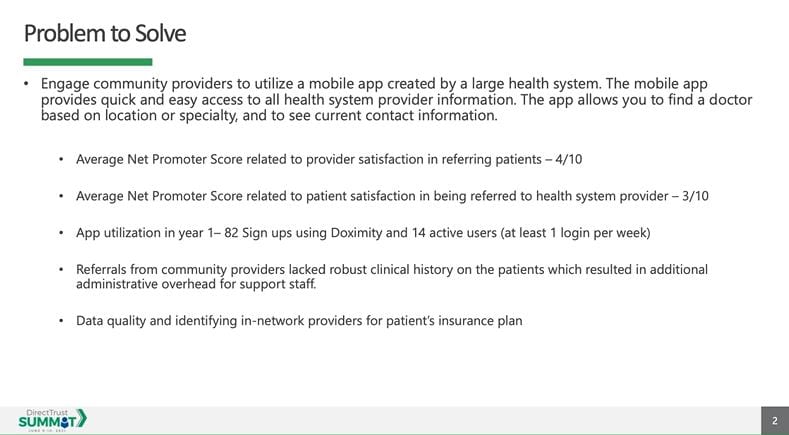
You can see by the Net Promoter Scores (NPS) that neither patients nor referring physicians were happy with the solution.
One of the many problems was the extra steps needed to get the patient’s clinical records from the referring physician to the health system. After the referral was made, the health system would have to call the physician’s office to request a copy of the clinical record. This placed a burden on the physician office staff and delayed the setting of appointments.
Based on this feedback the system made changes to the app, including implementing DIRECT Address and leveraging HIE data for patient history. The changes had a big impact:
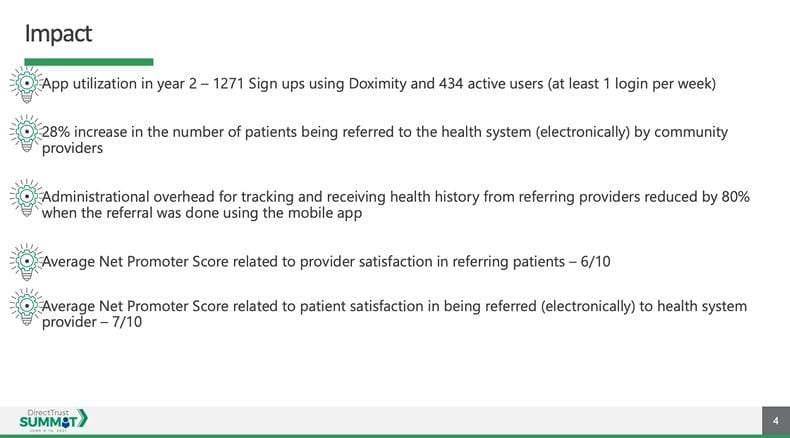 The improvement in NPS is impressive – and demonstrates how operational improvements made possible by the easy sharing of data can lead to an improvement in patient experience. By eliminating the unnecessary manual steps for patient record transfer, they made life easier for referring physicians and patients alike.
The improvement in NPS is impressive – and demonstrates how operational improvements made possible by the easy sharing of data can lead to an improvement in patient experience. By eliminating the unnecessary manual steps for patient record transfer, they made life easier for referring physicians and patients alike.
A fantastic Day 1
Day 1 of the #DirectTrustSummit was fantastic. The presentations were short and punchy, full of great information. Tripathi and Mathew got things started on the right foot and that carried through the rest of the day. I’m looking forward to Day 2.













