Since the start of the SARS-COVID-19 Pandemic forced most doctors to adopt remote options for scheduling and visiting with patients, telehealth has become the normal and acceptable method of patient encounters. However, that does not mean every doctor is prepared or properly trained to perform a telemedicine visit. I certainly did not receive training on how to do a virtual history and physical, a follow-up visit, or an acute visit during any point of my medical education. Fortunately for the doctors of tomorrow, we can better prepare them by establishing education around telehealth.
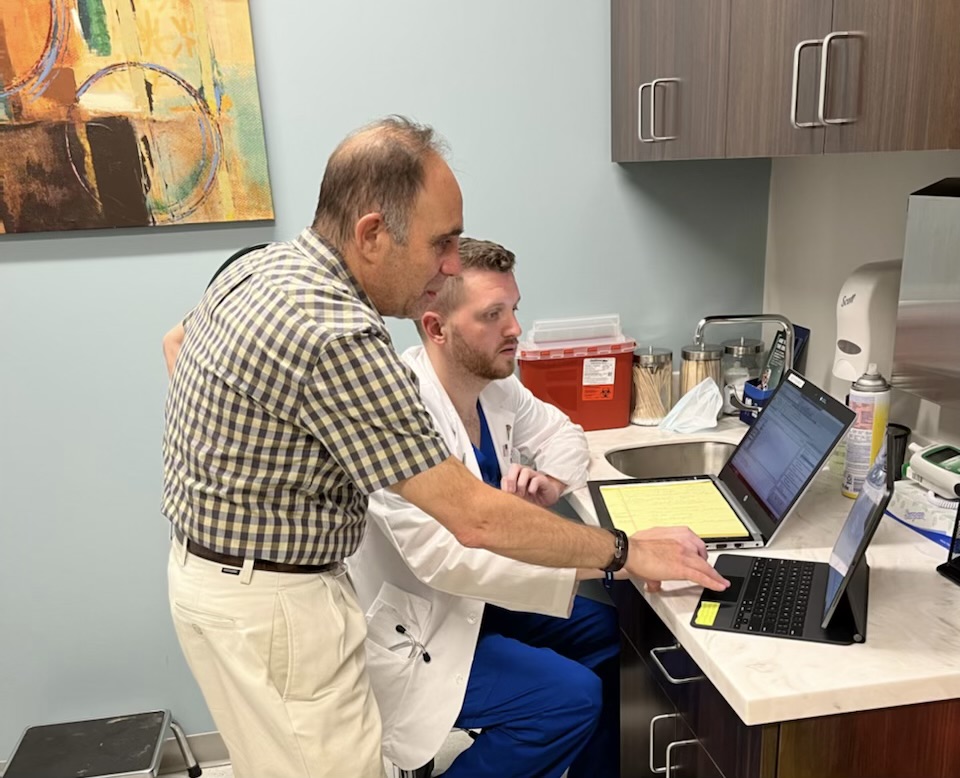
Thus, in our academic Family Medicine office, we are teaching fourth-year medical students how to perform telemedicine encounters. It is important to teach that these virtual visits are the same as in-person medical visits. They can be documented as such in the electronic health records and billed accordingly.
As a medical school, Philadelphia College of Osteopathic Medicine (PCOM) is uniquely positioned to support our Family Medicine practice with students who are not only eager to acquire first hand training but are also digital natives able to easily navigate new technology. With virtual meeting technology poised for continued growth, telemedicine has secured its place as a necessary tool to help improve access to care and deliver services to more patients.
In addition to the scope of Family Medicine, PCOM also includes interprofessional education (IPE), involving students and faculty from the Schools of Psychology, Physician Assistant, along with D.O. students. One example from PCOM is a previous presentation that included an interaction between a patient and doctor via a real-time (synchronous) video encounter. The patient was able to connect with both the physician and psychologist in collaboration to offer better coordination of care.
In our PCOM Family Medicine office, we set up our telemedicine visits in a similar fashion to in-person visits. First, the patient is contacted and the connection is established. The patient is then registered remotely through the phone before being triaged, when possible, with chief complaint, history of present illness, and available vitals. The vitals are gathered through remote patient reporting when possible. This can include the patient’s weight, home blood pressure, heart rate, pulse oximetry, and a finger stick glucose level. The medical student can then access the digital platform to review the electronic medical record (EMR) before using a separate tablet to start the encounter. The platform used by PCOM and our students is Doxy. me. The student learns that a real-time video telemedicine visit requires the same elements of proper documentation of a history and physical exam as its in-person counterpart. The student is taught that many key physical exams can be performed in a remote setting. Such as: constitutional (mild vs acute distress, anxiousness, etc.), HEENT (normocephalic, atraumatic, lesions, etc.), neck vein distention, use of accessory respiratory muscles, respiratory effort, alertness, focal deficits (puffing of cheeks), ambulation (assistant to patient may hold the common smartphone), orientation, and so on.
Thus, with the waxing and waning of the current pandemic, patients are not only accustomed to, but many times prefer the telemedicine visit. Medical offices must capture these encounters and continue the care which is at risk without access. The sooner we train our medical students, the more comfortable and adept they will be performing these visits.
Larry Finkelstein DO, FACOFP
Dr. Larry Finkelstein is a Professor at Philadelphia College of Osteopathic Medicine, department of Family Medicine.Dr. Finkelstein has teaching responsibilities in bioethics, oncology, geriatric medicine and primary patient care. He is also course preceptor for the 4th-year urban health care rotation. An active practitioner and lecturer, Dr. Finkelstein has made several presentations to senior citizens’ groups on reducing the risk of heart disease, heart attack warning signs, and stroke prevention. Dr. Finkelstein received his D.O. from PCOM in 1987 and completed his internship and residency within PCOM’s network at the St. Agnes Medical Center, focusing on general practice.


Comments are closed