The first article in this series laid out what we know about body weight and obesity today. The rest of the Lean Digital series will look at some contributions that digital technologies are making toward solutions.
The best contribution that information can make to weight management is to find more effective, personalized treatments: to match the right person to the right treatment, whether it be surgery, drugs, diet, exercise, or some combination. AI is turning up intriguing successes in this endeavor.
I talked to Dr. Ronald Razmi, co-founder and managing director at Zoi Capital and author of the book AI Doctor: The Rise of Artificial Intelligence in Healthcare.
On the scale between automation and human intervention, Razmi is firmly on the side of the “human touch.” He says that the relationship between the care manager and the patient is the number one driver of success. But he approves of wearables to monitor people “in their natural habitat” and using data to personalize treatments.
Razmi identifies two general contributions of AI. First, it can accelerate research into genetics, microbiomes, and other factors to come up with a treatment plan. Second, AI can pull together medical data from disparate sources to create a unified patient record.
Genetics, Phenomics, and Biomarkers for Weight Gain
Razmi’s first approach characterizes the work of Dr. Andres Acosta, who did research into obesity biomarkers for years at the Mayo Clinic. He then cofounded Phenomix Sciences to commercialize their findings and allow them to be used “anywhere in the world.” He wants to move weight “from stigma to biology.” Not only does he hope to solve people’s weight problems; he wants to explain to them how they got where they are biologically.
Not every obese person has the same problem, he says. Machine learning on biomarkers turned up 11 different classes of obesity—but that’s a rather complex classification. The researchers “took it out of the black box” and found that many of the classes had dimensions in common. Ultimately, they reduced the classes of obesity to four phenotypes, which were tested in a study:
- Hungry Brain: These people keep on eating because they don’t feel full, when others would. The solution includes intermittent fasting and eating a large volume of low-calorie foods such as salads.
- Hungry Gut: These people eat between meals, because something is telling the brain that the body needs something to digest. Treatment includes giving a protein hormone after each meal.
- Emotional Hunger: These people are using food compulsively to cover up negative emotions or feel a reward. The treatment is behavioral therapy.
- Slow Burn: These people might or might not be overeating, but the calories are not metabolized by the body and end up as fat. The treatment is exercise.
Biomarkers can also predict one’s response to medications. The Mayo team found some older drugs (which are cheaper than GLP-1 medications and have fewer side effects) that were rejected as ineffective, but that actually work on an impressive 30%-40% of patients.
If genetics lie at the basis of obesity, the patient is more likely to gain weight back after bariatric surgery.
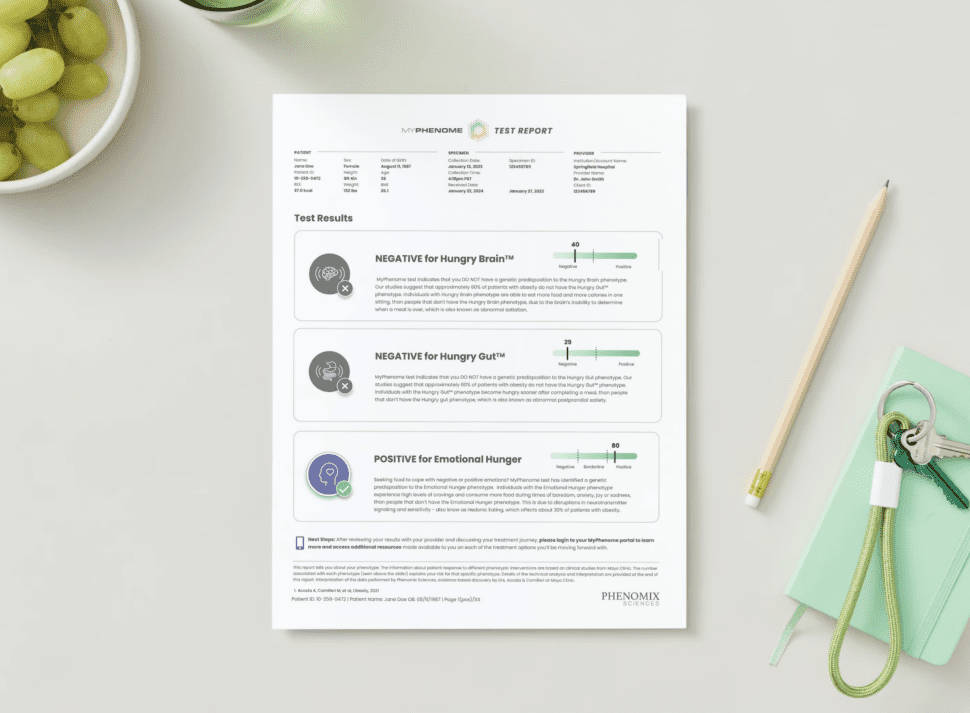
Phenomix Sciences has marketed the MyPhenome Test to determine biomarkers and recommend treatments (Figure 1). Participants in the program in one study lost 8% of their weight in 12 weeks, compared to 4% in the control group.
Personalized and Holistic Behavioral Recommendations
OM1 illustrates an AI-driven approach to analyzing data from many sources. OM1 estimates risks and personalizes treatment recommendations by running large amounts of data on each patient through AI models. Their technology is based on real-world data from hundreds of millions of patients. NLP can extract details such as what treatments the patient has already tried, and their reactions.
Patients are evaluated on the contents of the EHR, pharmacy data, and claims data.
Like many companies profiled in this series, OM1 is holistic. They want to treat not just obesity or diabetes, but related comorbidities such as sleep apnea. Dr. Joseph Zabinski, their VP, head of commercial strategy & AI, says it’s important to decide what to treat. For some people obesity might be the chief complaint, whereas for others it might be diabetes, depression, or something else.
They also emphasize the interaction between mental and physical health. This interaction is still underestimated in most of the medical field, Zabinski says. He points out that some drugs might solve one problem but make depression or anxiety worse; on the other hand, a depression medication can lead to weight gain.
Besides injecting recommendations into the physician workflow, OM1 can do population-level studies and predictive modeling, where they identify people who might benefit from targeted treatment.
DarioHealth has been offering a digital solution for behavioral health for more than a decade. They, too, try to be holistic, according to Dr. Omar Manejwala, chief medical officer. At the start they might be treating obesity, but the solution can switch according to the patient’s needs and concentrate, say, on improving depression or back pain. AI is used in a modest way to match each person to the proper user journey.
Studies document Dario’s effectiveness for weight loss and diabetes, for reducing health care costs, and for cutting hospital readmissions.
A “whole person profile” is also important at apree health, according to CEO Donald Trigg. They can, for instance, flag when a drug might be inappropriate because of side effects or adverse interactions.
The company describes itself as “the first integrated health network that combines data-driven personalization, a coordinated care model, and aligned incentives,” and employs coaches certified by the National Board for Health and Wellness. Thus, they stress the human side of health care, striving to “create a durable primary care relationship” for behavioral health and care management. A blog posting lists their effects on improved outcomes.
Data points that they measure include the usual vital signs (blood pressure, A1C, etc.) along with other HEDIS metrics and related factors such as eye and kidney health, cancer screening, and depression.
In this article, we’ve seen a few uses for AI in weight treatments. Some verge on behavioral health. There will be a lot more on behavioral health as this series continues. The next article introduces the support that digital apps and services offer for behavior change.














Add Comment