Virtual healthcare refers to delivering healthcare services remotely, using telemedicine, telehealth, and e-health. These technologies allow healthcare providers to communicate with patients, diagnose and treat conditions, and provide ongoing care through virtual, rather than in-person, visits.
Virtual healthcare has several benefits. It can increase access to care, especially for people living in rural or underserved areas or those with mobility issues. It can also reduce the burden on traditional healthcare systems by allowing patients to receive care from the comfort of their own homes and reducing the need for in-person visits. Virtual healthcare can also improve the efficiency of the healthcare system by enabling providers to see more patients in a shorter time.
Virtual healthcare can include other virtual services, such as online consultations with healthcare providers, virtual support groups, and online self-care resources. Virtual healthcare is expected to grow in the coming years as more people turn to technology to access healthcare services. In this article, we explore the pros and cons of virtual healthcare and inform the reader about the benefits of remote patient monitoring, an innovative, cutting-edge form of virtual healthcare.
What is Virtual Healthcare? How Does it Work?
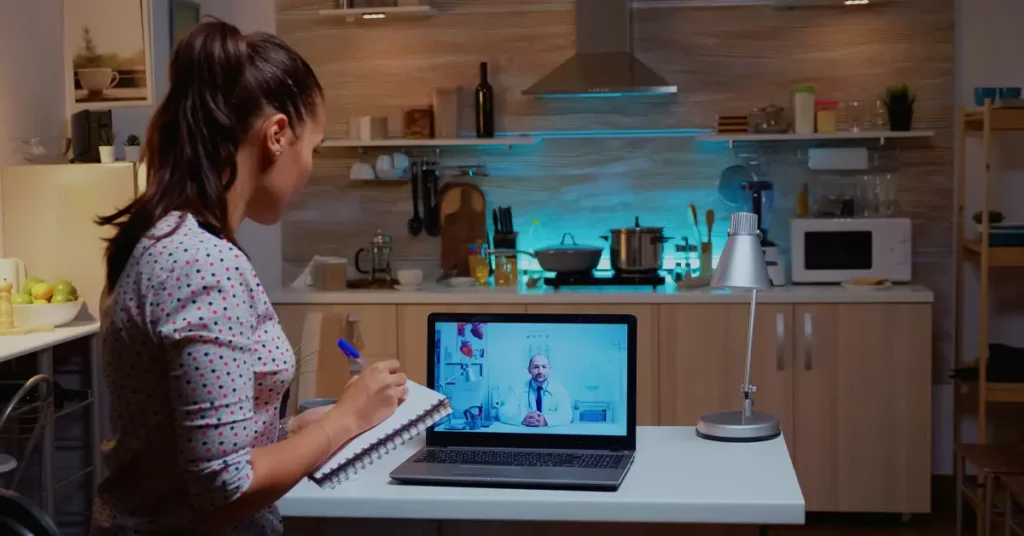
Virtual healthcare can be accessed through various platforms, including phone, video, email, and online portals. Telemedicine, a type of virtual healthcare, involves using video conferencing or other electronic communication methods to connect patients with healthcare providers. This can be done through a computer, smartphone, or another device with a camera and internet connection.
During a virtual healthcare visit, the patient and provider can discuss the patient’s symptoms, medical history, and other relevant information. The provider may also perform a physical examination, if necessary, remotely using digital tools such as a stethoscope or otoscope that the patient can use from their homes, for example. The provider can then diagnose the patient’s condition and recommend a treatment plan, including prescription medications, lifestyle changes, or referrals to specialists.
Virtual healthcare can be used for various conditions, from minor ailments to chronic diseases. It is beneficial for conditions that can be effectively managed remotely, such as high blood pressure, diabetes, and mental health issues. Virtual healthcare can also be used for follow-up appointments, medication management, and ongoing care.
Overall, virtual healthcare is a convenient and efficient way for patients to access healthcare services while reducing the burden on traditional healthcare systems. It has the potential to improve the quality of care and increase access to care for people living in rural or underserved areas or those with mobility issues.
What is Telehealth? How Does it Work?
Telehealth, which is one example of virtual healthcare, refers to using electronic communication technologies to provide healthcare services remotely, such as telephone, video conferencing, and online portals. It is a type of virtual healthcare that allows patients to receive care from the comfort of their own homes or other locations rather than having to visit a healthcare facility in person.
Telehealth can be used for many healthcare services, including consultations with healthcare providers, diagnoses and treatment of conditions, and ongoing care management. It can be accessed through various platforms, such as a computer, smartphone, or another device with a camera and internet connection.
During a telehealth visit, the patient and healthcare provider can discuss the patient’s symptoms, medical history, and other relevant information. The provider may also perform a physical examination, if necessary, using digital tools such as a stethoscope or otoscope. The provider can then diagnose the patient’s condition and recommend a treatment plan, including prescription medications, lifestyle changes, or referrals to specialists.
Telehealth is beneficial for managing chronic conditions, such as diabetes, high blood pressure, and mental health issues, as well as follow-up appointments and medication management. It can also provide care for minor ailments, such as cold and flu symptoms, skin rashes, and other conditions that can be effectively managed remotely.
Telehealth is a convenient and efficient way for patients to access healthcare services while reducing the burden on traditional healthcare systems. It has the potential to improve the quality of care and increase access to care for people living in rural or underserved areas or those with mobility issues.
How is Virtual Healthcare Different from Telehealth?
Virtual healthcare and telehealth are often used interchangeably, but they are different. Virtual healthcare refers to delivering healthcare services remotely, using various technologies such as telemedicine, telehealth, and e-health. On the other hand, Telehealth refers explicitly to using electronic communication technologies, such as telephone, video conferencing, and online portals, to provide healthcare services remotely.
One key difference between virtual healthcare and telehealth is the types of services they provide. Virtual healthcare encompasses a wide range of services, including telemedicine, and other virtual services, such as online consultations with healthcare providers, virtual support groups, and online self-care resources. Telehealth, on the other hand, is explicitly focused on providing healthcare services through electronic communication technologies.
Another difference between virtual healthcare and telehealth is the platforms they use to deliver care. Virtual healthcare can be accessed through various platforms, including phone, video, email, and online portals. Telehealth, as a subset of virtual healthcare, is also accessed through electronic communication technologies, such as video conferencing or phone calls.
Overall, the main difference between virtual healthcare and telehealth is the scope of services they provide. Virtual healthcare is a broad term that includes telehealth and other virtual services, while telehealth focuses on providing healthcare services through electronic communication technologies.
What are the Benefits of Virtual Healthcare?
Virtual healthcare, which includes telemedicine, telehealth, and other virtual services, offers several benefits for patients and healthcare providers. By using technology to deliver healthcare services remotely, virtual healthcare can increase access to care, improve the efficiency of the healthcare system, and provide a more convenient and comfortable experience for patients. Some of the specific benefits of virtual healthcare include the following:
1. Increased Access to Care
With the advancement of virtual healthcare, more accessible healthcare for all has become a reality. For many healthcare needs, gone are the days of waiting for an appointment at the doctor’s office and then making a second trip for follow-up visits. This new technology transforms how patients receive and deliver healthcare, providing more efficient patient care.
Virtual healthcare can increase access to care, especially for people living in rural or underserved areas or those with mobility issues. It can also make it easier for people to receive care during the COVID-19 pandemic, as it allows patients to receive care from the safety of their homes.
One aspect of virtual health that significantly improves access, called Remote Patient Monitoring (RPM), provides enhanced access to healthcare through digital devices such as smartphones, tablets, and computers. RPM allows doctors and patients to monitor vital signs and other health indicators remotely, allowing doctors to make timely interventions when needed. It also enables easy sharing of essential information between providers, eliminating unnecessary paperwork and reducing costs associated with in-person visits.
2. Reduced Burden on Traditional Healthcare Systems
Virtual healthcare can reduce the burden on traditional healthcare systems by allowing patients to receive care from the comfort of their own homes and reducing the need for in-person visits. This can free up capacity in healthcare facilities and allow providers to see more patients in a shorter period.
Virtual healthcare allows patients to access healthcare services remotely, which helps reduce the demand for in-person appointments and frees up capacity in traditional healthcare settings. This can be especially useful during times of high demand, such as during a pandemic or other public health crises, when traditional healthcare systems may be overwhelmed.
Virtual healthcare can also reduce the burden on traditional healthcare systems by allowing patients to receive care for certain conditions without hospitalization. For example, patients with chronic illnesses or other conditions that require ongoing monitoring may receive care through virtual healthcare services, which can help reduce the need for hospital stays and the associated costs.
3. Improved Efficiency
Virtual healthcare allows patients to access healthcare services remotely, which helps reduce the need for in-person visits and the associated travel time and costs. This can be especially useful for patients living in rural or underserved areas or those who have difficulty accessing in-person care due to mobility issues or other factors.
Virtual healthcare can also improve efficiency by allowing providers to see more patients in a shorter time. For example, a healthcare provider can conduct several virtual appointments at the same time it would take to see a single patient in person. This can help reduce wait times and improve patient care access.
Finally, virtual healthcare can also improve efficiency by reducing the need for paperwork and other administrative tasks, as many of these tasks can be completed electronically. This can free up time for healthcare providers to focus on patient care and can help to improve the overall efficiency of the healthcare system.
Overall, improved efficiency is one of the benefits of virtual healthcare, as it can help to reduce wait times, improve access to care, and reduce the administrative burden on healthcare providers. More convenient and comfortable experience for patients.
4. Convenient and Comfortable Experience for Patients
Virtual healthcare can provide a more convenient and comfortable experience for patients, as it allows them to receive care from the comfort of their own homes. It can also be more convenient for patients who have busy schedules or limited availability for in-person visits.
Virtual healthcare allows patients to access healthcare services remotely, so they do not have to travel to a healthcare facility or wait in a waiting room. This can be especially useful for patients living in rural or underserved areas or those who have difficulty accessing in-person care due to mobility issues or other factors.
Virtual healthcare can also be more convenient for patients who have busy schedules or have difficulty taking time off work or other commitments to attend in-person appointments. By providing an alternative means of accessing care, virtual healthcare can help to make healthcare more accessible and convenient for patients.
In addition to being convenient, virtual healthcare can also provide a more comfortable experience for patients by allowing them to receive care from the comfort of their own homes. This can be especially useful for patients who are anxious or uncomfortable in traditional healthcare settings or who have difficulty leaving their homes due to medical conditions or other factors.
5. Improved Quality of Healthcare
Utilizing virtual health, patients can obtain personalized solutions, and providers can consult with other specialists more easily. This enhances the precision of diagnoses and the efficacy of treatments. In 2020, the Hypertension Journal documented strong evidence that explicitly supports virtual care for remote monitoring, counseling, addressing the individual electronic health record, and communication regarding chronic illnesses like cardiovascular and respiratory diseases.
Since providers can access patients’ medical records online, they have everything they need to provide high-quality care. Improvements in outcomes like mortality, quality of life, mental well-being conditions, and fewer hospital admissions have been seen in some clinical outcomes.
6. Convenience for Patients and Providers
Virtual healthcare allows patients to visit their physician from the comfort of their homes and get a health diagnosis without them or their family members having to leave their houses. Plus, there’s no need to wait in long lines at the doctor’s office or sit in a cramped exam room. For doctors or nurses, it means they can see more patients conveniently in a day, saving time and treating more patients.
7. Efficient Management of Chronic Conditions
Virtual healthcare allows patients to obtain the necessary care and support without taking time off work or rearranging their schedules. Virtual care or virtual health is available 24/7, so patients can get help whenever needed. It is more affordable because patients do not need to travel to a clinic to receive treatment. For doctors, virtual or virtual primary care means more efficient chronic condition management based on the patient’s electronic health record. They can see more patients in less time to handle more cases overall.
8. Faster Solutions for Urgent Symptoms
For those with urgent issues, virtual healthcare can provide beneficial solutions and relief from their symptoms. As the demand for virtual health options increases, so does the urgency for new innovative solutions beyond offering convenience and cost savings. Urgent care centers now offer telemedicine visits and medication refills available 24 hours a day, seven days a week.
Digital tools like symptom checkers can help individuals quickly assess their condition before seeking professional help or making an appointment with an online doctor or telemedicine provider. Additionally, digital health records allow patients to access their medical history quickly and easily, which can be helpful when seeking urgent medical advice or dealing with emergencies.
9. Provides the Best Healthcare from Almost Anywhere, Any Time
Virtual healthcare allows patients to see a provider from the comfort of their living room or home while receiving high-quality healthcare. Virtual healthcare provides patients access to high-quality care from anywhere, allowing them to receive medical attention without traveling or disrupting their daily routines. This can be especially beneficial for people who live in remote areas, have mobility issues, or have difficulty accessing traditional healthcare facilities. Medical professionals are available from almost anywhere while receiving virtual primary or acute care.
10. Efficient Self-Care for Patients with Chronic Conditions
Virtual healthcare can be an effective tool for helping patients with chronic conditions manage their health and improve their quality of life. By providing patients with access to remote care, virtual healthcare can help patients better manage their chronic conditions, such as diabetes, heart disease, and asthma, without having to leave their homes.
Virtual healthcare can help patients better manage their chronic conditions by providing them with education, support, and resources. For example, it can give patients access to health coaches, dietitians, and other healthcare professionals who can help them develop a self-care plan and provide the tools and support they need to manage their condition.
Overall, virtual healthcare can be an effective tool for helping patients with chronic conditions have more control over their health and manage their needs more effectively. By providing access to remote care, virtual healthcare can help patients better manage their chronic conditions and improve their quality of life.
What are the Challenges of Virtual Healthcare?
While virtual healthcare has many benefits to health systems, it is not without its challenges. Many people are still hesitant to use it for health-related issues, so there is a need for some education and marketing to help convince them of its many tangible benefits. By being aware of these challenges and taking the necessary steps to answer and address them, we can make virtual healthcare a reality for everyone. Some of the challenges of virtual healthcare include the following:
1. Access to Technology
To participate in virtual healthcare, patients need access to the necessary hardware and software, such as a computer, tablet, or smartphone with a camera and reliable internet connection. If a patient does not have access to these resources, they may be unable to participate in virtual healthcare appointments or access other digital healthcare services.
Access to technology can also challenge virtual healthcare in areas with limited or unreliable internet coverage. Suppose a patient lives in a rural or underserved area. In that case, they may not have access to the high-speed internet connection needed to participate in virtual healthcare appointments or access other digital healthcare services.
2. Internet Connectivity
Virtual healthcare relies on a stable and reliable internet connection to facilitate communication and exchange of information between patients and healthcare providers. Suppose a patient cannot access a stable and reliable internet connection. In that case, it can be difficult for them to participate in virtual healthcare appointments or access other digital healthcare services.
Even if a patient has access to a stable and reliable internet connection, they may still face challenges if their connection is slow or has low bandwidth. This can make it difficult for them to participate in video appointments or access large files, such as medical records or diagnostic images.
Internet connectivity can also challenge virtual healthcare in areas with limited or unreliable coverage. Suppose a patient lives in a rural or underserved area. In that case, they may not have access to the high-speed internet connection needed to participate in virtual healthcare appointments or access other digital healthcare services.
3. Lack of Knowledge in Using the Technology
Virtual healthcare relies on technology to facilitate communication and exchange of information between patients and healthcare providers. Suppose the patient needs to become more familiar with the technology being used. In that case, it can be difficult for them to fully participate in virtual healthcare appointments, which may lead to misunderstandings or inadequate treatment.
Virtual healthcare often uses various digital tools and applications, such as telemedicine platforms, electronic health records, and wearable devices. Suppose a patient needs to gain knowledge in using these tools. In that case, they can properly use them to track their health, communicate with their healthcare provider, or access important information.
A lack of knowledge in using technology can also lead to difficulties accessing virtual healthcare services. For example, suppose a patient cannot navigate a telemedicine platform or lacks the necessary hardware or internet connection to participate in a virtual appointment. In that case, they may be unable to take advantage of the convenience and accessibility of virtual healthcare.
Healthcare providers should use the latest and greatest technology to provide patients with the best possible care. Healthcare providers should ensure they are training their staff on how to use these new tools and be proactive in answering any questions patients may have about virtual health or virtual healthcare.
With the DrKumo RPM solution, next-Generation RPM programs using digital tools come with user-friendly mobile apps that can analyze a patient’s overall health. DrKumo can assist patients with remote care to help improve their lifestyle or diet and their adherence to medication and treatment plans with the help of Bluetooth-enabled mote patient monitoring devices that securely communicate patient data to their providers.
4. Privacy and Security
Virtual healthcare involves collecting, storing, and sharing sensitive personal and medical information. If this information is not adequately protected, it could be accessed by unauthorized individuals, leading to potential privacy breaches.
Virtual healthcare often uses various digital tools and applications, such as telemedicine platforms, electronic health records, and wearable devices. If these tools are secure, they could protect the privacy and security of patients’ personal and medical information.
Virtual healthcare may also involve public internet connections or unsecured networks, which could expose sensitive information to hackers or other cyber threats.
Overall, privacy and security are important considerations in virtual healthcare, as they are essential for protecting the confidentiality and integrity of patients and medical information. With proper privacy and security measures, virtual healthcare may be viable for some patients.
5. Limited Physical Examination Capabilities
Virtual healthcare relies on communication and information exchange between patients and healthcare providers to diagnose and treat medical conditions. While virtual healthcare can effectively manage specific conditions, it may only be suitable for some medical issues, especially those requiring a physical examination. For example, if a patient has a rash or other physical symptoms that need to be evaluated, a virtual healthcare appointment may not be sufficient to diagnose the problem accurately.
Virtual healthcare may provide a different level of support and guidance than an in-person appointment. For example, a healthcare provider may not be able to assess a patient’s mobility or perform specific physical tests during a virtual appointment, which can limit their ability to provide an accurate diagnosis or treatment plan.
Finally, virtual healthcare may not be suitable for patients unable to communicate effectively due to language barriers, cognitive impairments, or other factors. In these cases, an in-person appointment may be necessary to accurately assess a patient’s health and provide the necessary care.
6. Reimbursement
Virtual healthcare is still a relatively new field, and many insurance providers may not cover virtual healthcare services or may only offer limited coverage. This can make it difficult for patients to afford virtual healthcare services and may discourage them from seeking care in this way.
Even if insurance providers cover virtual healthcare services, they may only reimburse at a different rate than in-person appointments. This can create a financial burden for healthcare providers who offer virtual healthcare services, which may limit the availability of these services.
Reimbursement for virtual healthcare services may vary depending on the specific service being provided, the location of the patient and provider, and other factors. This can create confusion and uncertainty for patients and providers and may make it difficult to determine their out-of-pocket costs for virtual healthcare services.
How Remote Patient Monitoring Helps Deliver Effective Virtual Healthcare
Remote patient monitoring (RPM) is a technology-based healthcare type that involves using digital devices and applications to collect and transmit patient health data remotely. RPM can be an effective tool for delivering virtual healthcare in several ways.
Firstly, RPM allows healthcare providers to collect and monitor patient health data remotely, which can help to identify potential health issues before they become more serious. This can be especially useful for patients at high risk for certain conditions, such as chronic illnesses or the elderly. By using RPM, healthcare providers can more effectively monitor these patients and intervene as needed to prevent complications.
Secondly, RPM can also help to improve the accuracy and effectiveness of virtual healthcare by providing healthcare providers with more detailed and up-to-date information about a patient’s health. For example, a patient’s vital signs, such as their blood pressure and heart rate, can be monitored remotely and transmitted to their healthcare provider, which can help to identify any potential issues or changes in the patient’s condition.
Finally, RPM can also help to improve the convenience and accessibility of virtual healthcare by allowing patients to receive care from the comfort of their homes. This can be especially useful for patients with mobility issues who live in rural areas or have difficulty accessing in-person care.
DrKumo is among the first companies to offer a highly secure, real-time remote monitoring solution that incorporates customizable disease management protocols (DMP). DrKumo has RPM devices that can measure and transmit the health data they collect to secure cloud storage, where healthcare providers can access the information whenever and wherever they choose. Some devices include pressure monitors, pulse oximeters, glucose meters, smart scales, electrocardiography (ECG) devices, and smartwatches.
Overall, remote patient monitoring can be a valuable tool for delivering effective virtual healthcare by helping to improve the accuracy and effectiveness of care and the convenience and accessibility of virtual healthcare for patients.
DrKumo, a Connected Health Technology Leader Provides the Best RPM Solution
DrKumo’s RPM solutions have been proven to dramatically improve patients’ overall healthcare by giving them more freedom to track and monitor their physiological data from home. These measurements provide their healthcare providers with more and better-quality vital information that equips them with the information they need to make the best, timely decisions for their patients. DrKumo’s RPM helps providers monitor the patient’s health remotely without having them physically present in the clinic or hospital setting. By obtaining real-time data from patients outside the clinic, healthcare providers can detect potential problems early on, providing an opportunity for timely interventions that could potentially prevent serious complications or hospitalization.
Conclusion
Virtual healthcare and telehealth are two terms used interchangeably to describe the use of technology for remote healthcare delivery. The main difference between virtual healthcare and telehealth is their scope of services. Virtual healthcare is a broad term used to refer to any healthcare service provided online, while telehealth focuses explicitly on delivering clinical services via online interactions. Remote patient monitoring (RPM) is integral to virtual health care and telehealth services and helps give patients more control over their health.
Learn more about our remote patient monitoring technology solutions and how they can benefit your practice. Contact us today!