The following is a guest article by Shaillee Juneja, Principal, & Shaun Sangwin, Senior Vice President, Business Development at Divurgent.

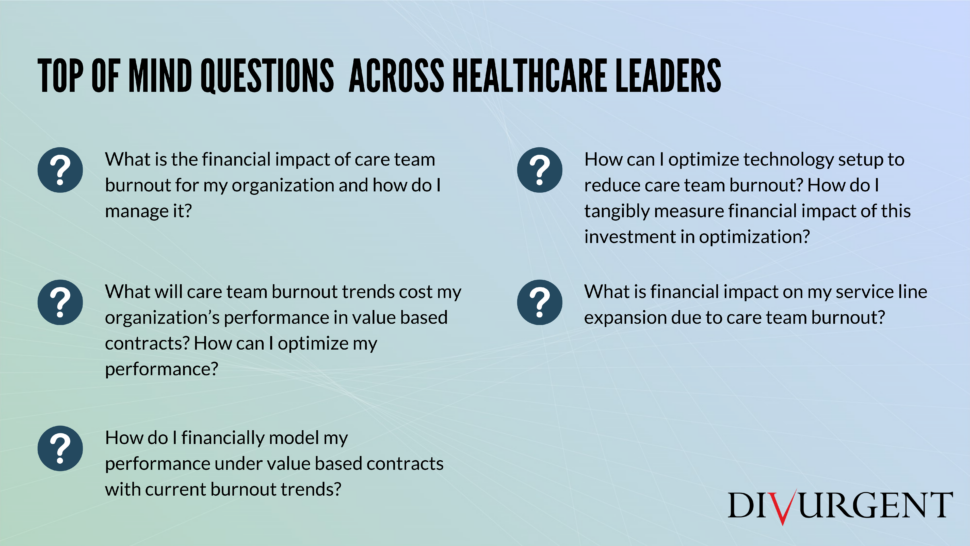
 Many, including the New England Journal of Medicine and the National Academy of Medicine, have described physician burnout as the “parallel pandemic,” but the problem is broader than provider burnout – it encompasses the entire care team.
Many, including the New England Journal of Medicine and the National Academy of Medicine, have described physician burnout as the “parallel pandemic,” but the problem is broader than provider burnout – it encompasses the entire care team.
Why? Because while the organizational cost of individual turnover of a nurse is less expensive than a physician, the impact on quality and patient satisfaction is significant. That impact has direct ramification on performance and reimbursement under a value-based care contract.
In short, you will be paid less if you have dissatisfied care teams under value-based care contracts.
In this article, we will talk about the magnitude of this problem and how leading organizations are deploying organizational changes to improve overall care team satisfaction.
 According to a 2020 KLAS Impact Report on Nurse Burnout, 25% of nurses and physician assistants are experiencing symptoms of burnout. Physician burnout remains a significant industry issue with a single turnover costing an organization anywhere from $250K to $1M (Bresnick, 2018).
According to a 2020 KLAS Impact Report on Nurse Burnout, 25% of nurses and physician assistants are experiencing symptoms of burnout. Physician burnout remains a significant industry issue with a single turnover costing an organization anywhere from $250K to $1M (Bresnick, 2018).
According to a 2016 National Healthcare Retention & RN Staffing Report, nursing burnout can lead to direct loses of $37,700 to $58,400 per turnover event or $5.2M to $8.1M annually for the average hospital. From a quality perspective, a 25% increase in nurse satisfaction is linked to an overall quality of care increase between 5% to 20%, according to an ANA’s National Database of Nursing Quality Indicators study.
As mentioned previously, this quality-of-care impact becomes increasingly important with the shift to value-based care. Despite the significance of nursing burnout to healthcare’s top and bottom line, many organizations lack a formal retention or satisfaction program for nurses.
With increasing acuity in hospitals and ambulatory centers, case mix index is going up dramatically, leading to more stringent provider/nurse to patient staffing ratios. Besides the changing dynamic of healthcare delivery, many organizational factors including communication, governance, and training can have a significant impact on overall care team satisfaction and burnout.
 Organizations that successfully deploy changes to improve the overall care team satisfaction take a multi-faceted approach that better align staffing/compensation to payment models, optimize technology and related processes, and include individual interventions that are tailored to the specific challenge areas or needs to that team member. Below, we outline some of the interventions across these domains:
Organizations that successfully deploy changes to improve the overall care team satisfaction take a multi-faceted approach that better align staffing/compensation to payment models, optimize technology and related processes, and include individual interventions that are tailored to the specific challenge areas or needs to that team member. Below, we outline some of the interventions across these domains:
Structural or organizational interventions
- Shift to optimal team-based staffing levels by leveraging predictive modelling techniques that show the financial impact of changes to care team composition for specific service
- Empower individuals with leadership
- Optimize workflows to enable nurses to practice at ‘top of license’ to reduce the documentation burden on
- Review and refine provider compensation model to align with new post-COVID volume projections and shifting payor mix.
Information Technology setup interventions
- Optimize your existing EHR governance and change management approach to create a culture of clinical/operations led improvements and a culture of collaboration towards a common goal.
- Provide enhanced technology training and communication using tools like eLearning, regular EHR update newsletters, and examples of how technology improves care quality, efficiency, access to care, or reduces costs.
Individual-focused interventions
- Combine EHR and other data sources to create a longitudinal view of care team EHR performance and tailor interventions (ex. training, EHR optimization, communication) to specific challenge areas of the individual.
- Invest in skills group and self-care program offerings for front line care team to help cope with the extra demands of the pandemic.
- Offer specialized therapy and mental health wellness programs for care team members to counter the impacts of burnout and create sustainability of performance.
- Create relaxation spaces within the work environment.
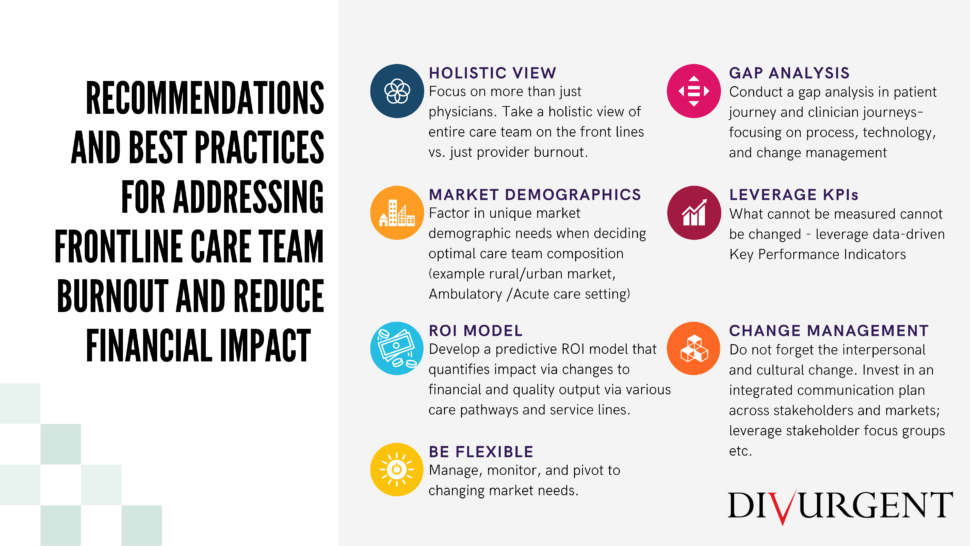 Organizations that understand and develop interventions associated with care team satisfaction and burnout will be the most successful over the coming decades as value-based care models become more prevalent. Existing care models and organizational structures do not support value-based care and as a result there are many untapped opportunities to prepare for this shift in payment models. One significant opportunity is the deployment of interventions focused on improving overall nurse satisfaction that, as a result, will improve patient care quality and reimbursement.
Organizations that understand and develop interventions associated with care team satisfaction and burnout will be the most successful over the coming decades as value-based care models become more prevalent. Existing care models and organizational structures do not support value-based care and as a result there are many untapped opportunities to prepare for this shift in payment models. One significant opportunity is the deployment of interventions focused on improving overall nurse satisfaction that, as a result, will improve patient care quality and reimbursement.
Citations:
Bresnick, J. (2018). EHR Users Want Their Time Back and Artificial Intelligence Can Help. Retrieved from HealthIT.
2020 KLAS Nursing Impact Report
About Divurgent
Divurgent is a solutions provider focused on what matters most to our client partners and is a proud sponsor of Healthcare Scene. We disrupt the typical value equation by using data-infused, flexible, and scalable solutions that demonstrate and quantify value for our partners.
We are committed to IT evolution, deploying tailored solutions that help our client partners achieve improved operational effectiveness, financial performance, and quality of customer experience. Throughout Divurgent’s 13-year history, we have experienced year-over-year growth measured in both revenue and employee headcount.
We take great pride in our private ownership and self-funded position. In an industry filled by capital infusion and acquisition, Divurgent is a rarity in today’s business climate. As a result of our private ownership, we can make decisions that are in the best interest of our client partners, rather than our shareholders. Learn more at www.divurgent.com