The fast-growing adoption of telemedicine and remote patient monitoring from the emergence of the COVID-19 pandemic led to hospitals and health systems launching new or expanding existing virtual care programs to accommodate a new reality for work-flow and patient care.
Now that the worst of the coronavirus acute impact is in our rear-view mirror, it appears medical care providers are reassessing these implementations and may “rip [out] and replace” those systems, according to The Great Shakeup, a survey report from Panda Health.
Panda Health collaborated with Sage Growth Partners to assess the perspectives of U.S. hospital and health system leaders in March 2023.
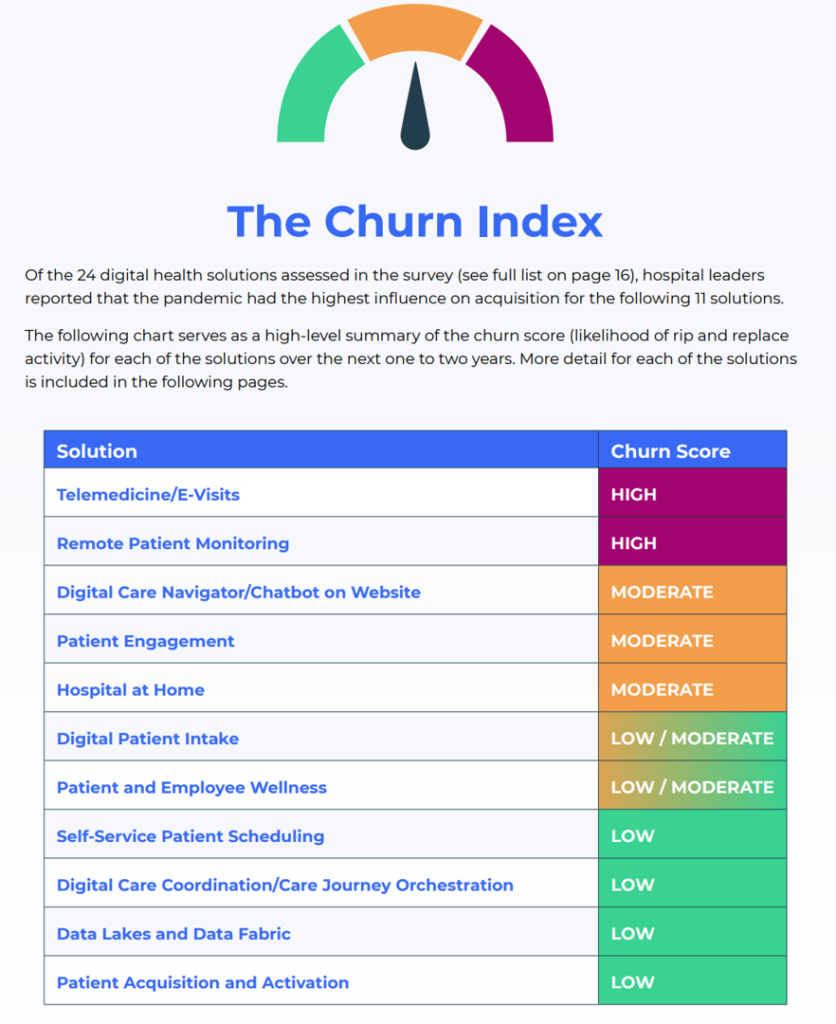
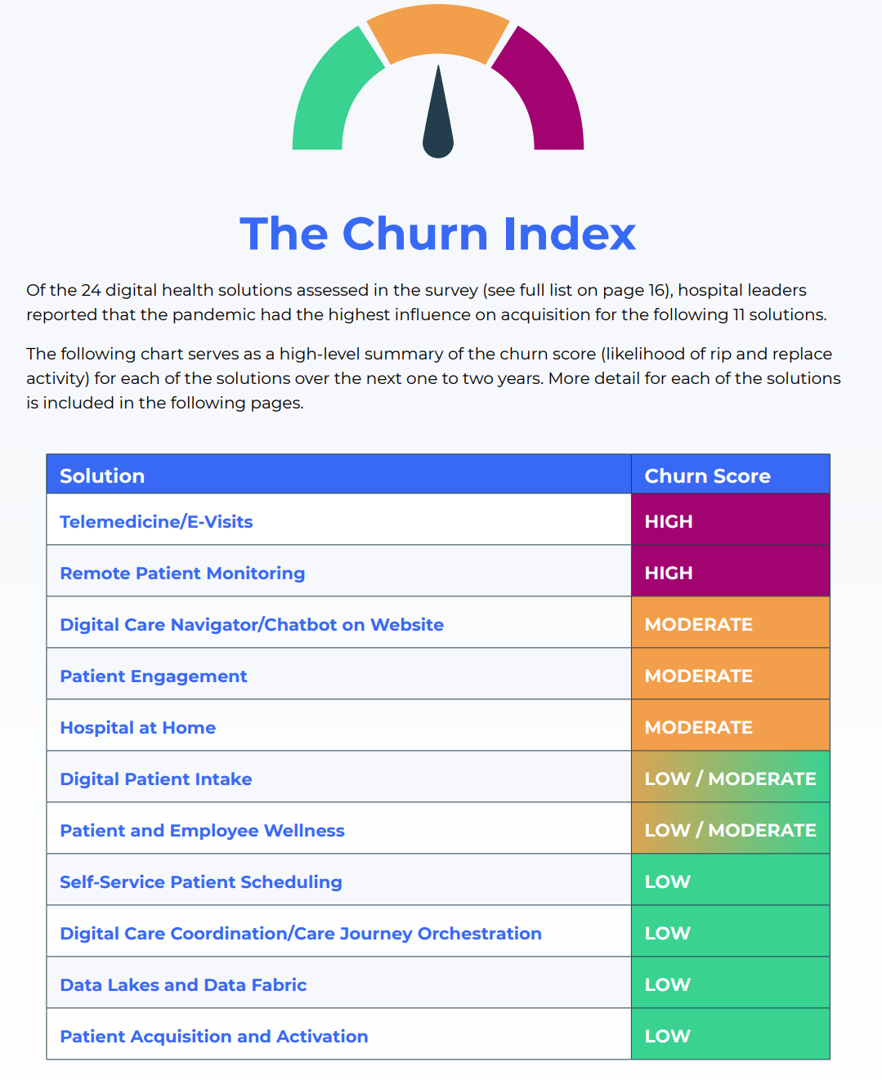
Based on this research, the team developed “The Churn Index,” a heat map/thermometer arraying which of 24 digital health solutions would be likely to be replaced in the coming months.
The top two areas fetching the “high” churn scores were telemedicine and e-visits, and remote patient monitoring, shown in the table from the report.
Telehealth was one of the most-influenced digital health adoption category in the pandemic, noted by 97% of providers.
For remote patient monitoring, 82% of hospitals deployed RHM since the pandemic emerged, with 19% of health systems adopting remote monitoring in the past 12 months (March 2022-23).
Panda Health points out that while they expect “high” churn for these two categories of digital health deployments, there will also be an increase of providers acquiring these solutions for the first time.
At the low-end of churn, we see self-service patient scheduling, digital care coordination, data lakes and data fabric, and patient acquisition and activation.
Moderate-to-low churn is seen for digital care navigation (including chatbots), patient engagement, hospital at home, digital patient intake, and patient and employee wellness.
For companies and technology developers serving digital health markets, it’s “time to brace for impact” as hospitals and health systems re-consider their fast-pivots to digital front doors and the migration of medical services from hospital-to-home during the pandemic, Panda Health recommends.

Health Populi’s Hot Points: “Are the best days of telemedicine behind us?” asks the first sentence in a Harvard Business Review essay on How to Tap the Full Potential of Telemedicine in Harvard Business Review (published June 6, 2023).
The article’s writer-team tells us the best days aren’t behind us, but…our concerns are understandable.
What would mitigate the risk would be, they say, for “the next level of virtual care [to] be reached if we bring more elements of the clinic to the patient.”
How to make this happen? Look to connected medical devices, such as consumer-facing and well-designed blood pressure monitors, blood glucose trackers, connected weight scales, and other digital health tools. Wearable tech such as the Apple Watch (which recently announced the watchOS 10 update with lots of health/care developments), as well as direct-to-consumer lab testing via at-home mail-in test kits (think: EverlyWell, Nurx, and LetsGetChecked as examples) and mobile diagnostic services that travel to patients’ homes for blood draws or imaging added to the health/care-at-home toolkit.
The authors also point to implanted technologies such as pacemakers and defibrillators for heart patients can keep patients connected with cardiologists and other health care providers monitoring conditions virtually — “separating data collection from the visit itself,” the essay explains. This frees up the clinician’s time to see patients in-person that need that kind of face-time versus diagnostic check-ins between major visits.
“New technologies and care approaches are pushing the frontier, not just of virtual visits but also of health care as a whole,” they conclude.
But technology itself isn’t the panacea — we must attend to design factors such as ease-of-use as well as design-for-equity and -privacy. 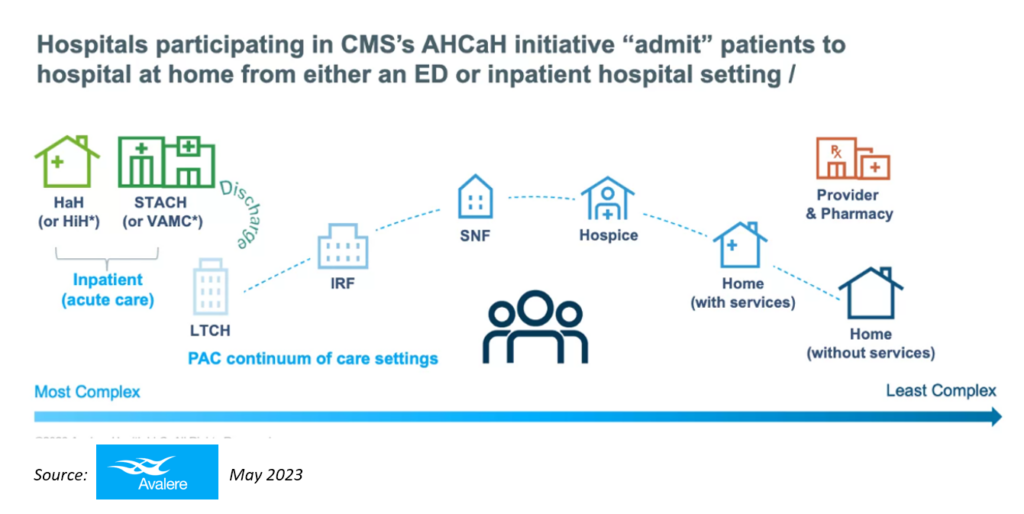
I’m encouraged working on this evolving ecosystem for health which is the New Home Care centered on peoples’ values and value.
We’re imagining and deploying new models for care delivery, such as the CMS AHCaH initiative which is part of the CMS Acute Hospital Care at Home reimbursement model that will see funding through the Consolidated Appropriations Act of 2023 through the end of 204. You can see a graphic for the concept here from Avalere’s excellent analysis of the state of Hospital at Home developments.
While this is a Hospital at Home model, but we will be growing Care at Home across the continuum funded in both private/commercial and public health insurance plans, from staying well and getting well to more acute care flows from/at home — enabled through consumer-enchanted digital health tools, baking in privacy- and equity-by-design.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.