Why AI matters
Healthcare organizations are hot on the trail of digital transformation. At the height of the pandemic, providers scrambled to digitize care (e.g., enabling telehealth visits). Since then, many are focused on using digital technologies to change the way they do business (e.g., adopting a hybrid care model).
Artificial intelligence (AI) is one of these groundbreaking technologies. Because AI uses machines to do tasks that traditionally require human intelligence (e.g., data analysis), it empowers providers to be smarter, faster, and more efficient in their care delivery. These enhancements have the potential to not only reduce provider costs, but also prevent errors, advance treatments, and improve health outcomes.

AI’s superpower lies in its ability to intelligently mine insights from the exponential amount of health data that is generated every second. Currently, the healthcare industry generates 30% of the world’s data volume. Even greater amounts of data will pump through the healthcare ecosystem with the proliferation of medical wearables, ingestibles, implantables, sensors and the Internet of Medical Things (IoMT).
Three out of four C-suite executives believe that if they don’t scale AI in the next five years, they risk going out of business entirely.
By 2025, the compound annual growth rate of healthcare data will reach 36%—6% faster than manufacturing, 10% faster than financial services, and 11% faster than media and entertainment. To make sense out of this data tsunami, AI is critical.
AI types and use cases
Before they can maximize AI’s value, healthcare executives need to fully understand and appreciate how it can help them. This requires acquiring a baseline knowledge of the AI concepts, challenges, and considerations.
There are five general types of AI.
Machine learning
Machine learning (ML) provides systems with the ability to think and act with less human intervention. ML scans structural (column-and-row) data, identifying patterns and using them to form educated judgments. Over time, as ML continues to learn from data, it becomes more self-reliant; its judgments become more accurate.
Generative AI is a form of ML that produces text, video, images, and other content based on a training data set.

Deep learning
A more sophisticated subset of ML, deep learning (DL) gives systems the ability to think using structures modeled on the human brain’s neural networks. Typically, DL needs less ongoing human intervention than ML. Also, it can analyze images, videos, and unstructured data in ways ML can’t easily do. However, it takes tremendous volumes of data to feed and build a DL system.

To achieve their growth objectives, 84% of C-suite executives believe they must leverage AI
Natural language processing
Natural language processing (NLP) gives systems the ability to understand human language as it is spoken and written. Using NLP, computer programs can translate text from one language to another, respond to spoken commands, and summarize large volumes of text quickly.

Computer vision
Computer vision trains computers to interpret and understand the visual world. Using digital images from cameras, videos, and deep learning models, machines can accurately identify and classify objects and then react to what they see.

Explainable AI
Explainable AI (XAI) is AI programmed to describe its purpose, rationale, and decision-making process in a way an average person can understand. By helping organizations understand an AI model’s behavior, XAI uncovers potential issues with the algorithm, such as AI biases. This transparency builds trust between users and the system, as it helps users to understand why and how a given model makes specific decisions.

AI regulations
In the United States, federal regulations generally focus on protecting patients, given the private and sensitive nature of each individual’s data. However, regulations exist to validate that AI algorithms are clinically robust and safe to use.
The FDA has approved more than 500 AI and machine learning models for medical use—most of which are in radiology. Most likely, this number represents a fraction of the tools being used today.
Under the 21st Century Cures Act, many AI tools are exempt from FDA regulation, as long as healthcare providers can independently review the basis for the medical recommendations and don’t rely on the technologies to make diagnostic or treatment decisions.
In December of 2023, the Department of Health and Human Services (HHS) struck first in regulating new AI tools in healthcare. The final HTI-1 rule, designed to advance healthcare interoperability and algorithm transparency, aims to help providers, hospitals, and physician groups choose safer, unbiased AI. The regulations, which were issued by the Office of the National Coordinator for Health IT (ONC), apply to clinicians using HHS-certified decision support software by the end of 2024. AI models that fall under this regulated umbrella are those used to analyze medical imaging, generate clinical notes, and alert clinicians to potential patient risks.
As conversations about AI ethics and responsible AI gain more traction, industry watchers expect health-related AI legislation to accelerate.
AI reimbursement
Medicare and Medicaid are beginning to reimburse for AI applications on a per-use basis, though adoption is still in its infancy. This is unique to healthcare; organizations in other industries have to pay for AI themselves.
Primarily, CMS covers AI reimbursement with AI-specific Current Procedural Terminology (CPT) codes created by the American Medical Association CPT Editorial Panel or by establishing New Technology Add-on Payments (NTAPs) for AI devices.
NTAP payments, which are part of Medicare’s Inpatient Prospective Payment System (IPPS), deliver additional reimbursements to hospitals above the standard Medicare Severity Diagnosis-Related Group (MS-DRG) payment amount for new technologies that raise a provider’s cost of treating an illness episode above the exiting episode-based payment and that provide a “substantial clinical benefit.”
CMS has also established new CPT codes for each use of specific AI devices. Typically, healthcare organizations use these codes when billing for AI services used in outpatient care, but they can be used to see reimbursement for inpatient care as well.
CPT code reimbursement is often determined based on Relative Value Units (RVUs) assigned under the Medicare Physician Fee Schedule, which is comprised of resource costs associated with physician work, practice expenses, and liability insurance.
While direct reimbursement AI technology remains limited, AI can nevertheless be successfully integrated into other existing payment models.
AI adoption success factors
According to research from McKinsey & Company analysts and Harvard University Economics professors, six factors contribute to a healthcare organization’s successful AI adoption.
- A mission-led roadmap to ensure a clear view of the one or two domains where AI’s value will be realized and a sequenced roadmap to get there
- Talent to ensure the right skills and capabilities are available to execute and innovate
- Agile delivery using pilots to introduce new approaches and to demonstrate progress and outcomes worthy of additional funding
- Technology and tools that are flexible, scalable, secure, and resilient to avoid overstressing systems with massive AI data compute activities
- Data management with a CXO-level data team that designs a data architecture that supports the broadest set of use cases (including unstructured data) and embeds risk management mechanisms
- An operating model change that leverages cross-functional teams to develop formal AI governance, orchestrate change management, and achieve workflow integration and algorithm development
When adopting technologies such as AI, the highest performers across industries spend 30–60% more than others and expect to increase their budgets by 10–15%. In particular, organizations with successful AI deployments generally overinvest in core technology architecture and data systems—often redesigning their tech stacks and mapping out the future state of their architecture.
AI and the cloud
To handle the large data volumes required to train and deploy AI models at scale, many providers point to the cloud as their go-to computing service. Because the cloud delivers servers, storage, databases, and software over the internet, it’s an attractive alternative to investing in and maintaining a physical IT infrastructure. The cloud also enables organizations to access its resources on demand and pay only for what they use.
AI chip scarcity
The major AI boom—fueled by the insatiable demand for running large language models—is applying pressure on the limited number of specialized chips, such as graphic chips (or GPUs) from Nvidia. GPUs are better-suited for AI, as they can run many computations simultaneously.
However, much of today’s cloud footprint runs on servers that use general-purpose CPU chips, which handle fewer computations at the same time and are less suitable than GPUs, which can support large, collaborative AI workload clusters.
However, cloud hyperscalers are quickly building out their AI infrastructure to meet rising demand.
Clinical data barriers
The cloud may help satisfy AI’s infrastructure needs, but healthcare organizations must also tackle data management—a significant challenge that 72% of Chief Data Officers say prevents them from scaling AI use cases.
For 97% of providers, ingesting real-time clinical data is crucial to their cloud use cases. Yet, only 3% haven’t encountered any challenges with streaming this data into the cloud. The main hurdle is the lack of internal resources to manage the data ingestion.
To stream clinical data into the cloud, it must first be translated from legacy standards (HL7v2, CD, X12, and DICOM®) to HL7® Fast Healthcare Interoperability Resources (FHIR®). Once clinical data is in FHIR, it’s easier to connect that data with a variety of cloud services and applications. (A FHIR store can also help providers capitalize on the cloud’s full potential.) Organizations that lack the technical resources to transform their healthcare data often rely on seasoned integration partners who are fluent across both legacy and FHIR standards. With the proper expertise, providers can execute projects on time and on budget. However, top-tier integration partners do more than tackle one-off data transformation projects. Rather, they build a reusable and scalable infrastructure that can transform data for future cloud use cases, which accelerates any integration’s time to value.
AI costs
When calculating AI’s ROI, providers should consider more than a vendor’s deployment costs. They should also factor in ongoing licensing fees as well as expenses for data processing, storage, and management.
In addition, providers should incorporate their internal organizational costs stemming from time, lost productivity and workflow interruptions for key staff, including administrative/project management, clinicians, data/ML engineers, and other IT support. Internal costs vary, depending on the AI type deployed, system customization, implementation scope, and project duration.
AI’s net savings for U.S. hospitals
In 2023, experts from McKinsey & Company and Harvard University published their estimates of AI’s financial impact on multiple healthcare stakeholders, including hospitals.
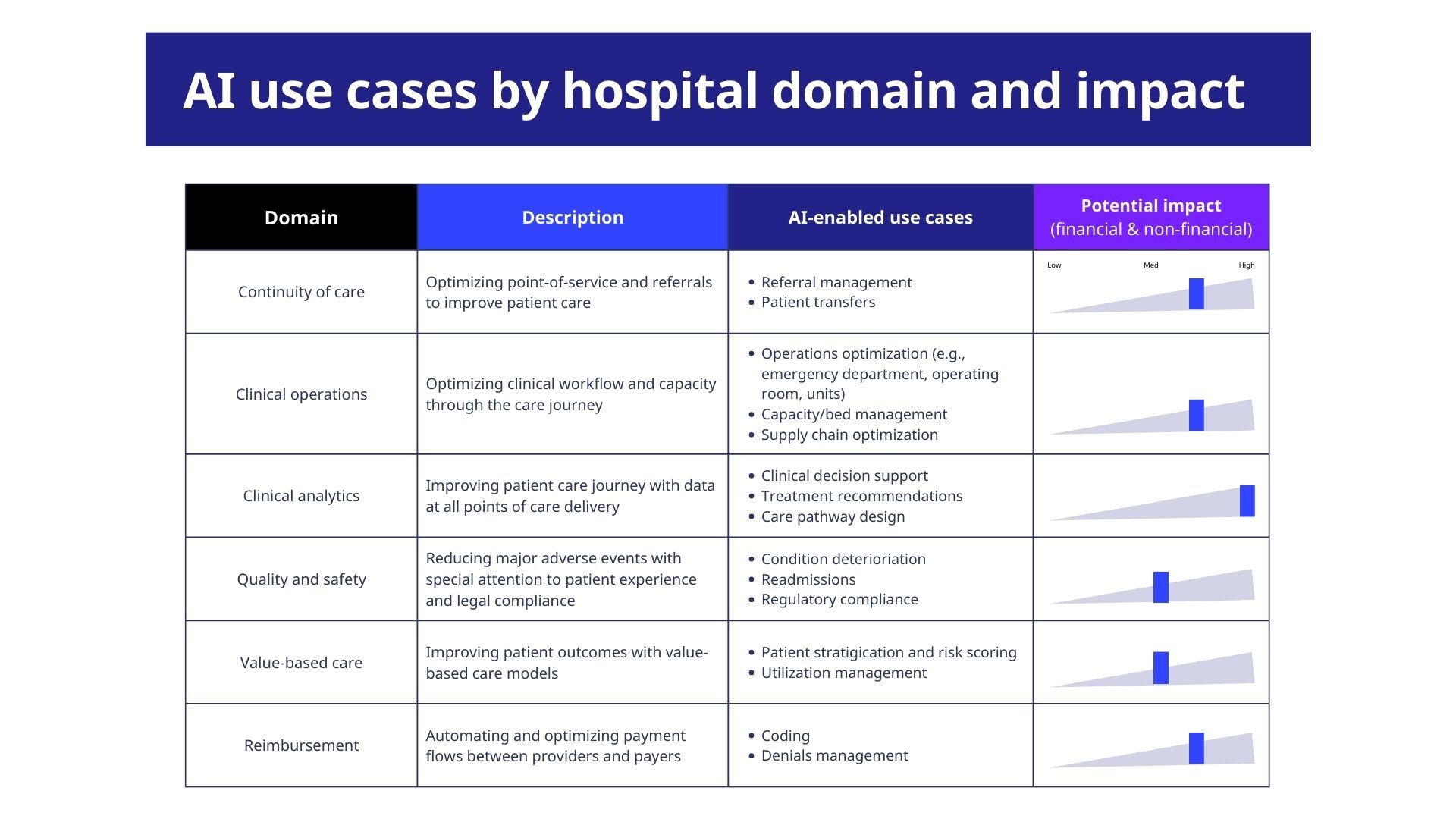
Using McKinsey’s proprietary value pool data, they calculated the total net savings that AI could feasibly generate for U.S. hospitals. They arrived at $60B–$120B total net opportunity across all hospital domains (or functional areas) within five years.
Stay in the know! Subscribe to our newsletter.
Sources
Adams, Katie. “Seven AI Pitfalls That Hospitals Should Avoid.” MedCity News, 21 Sept. 2023.
“Artificial Intelligence.” Accenture, www.accenture.com. Accessed 3 Oct. 2023.
Bousquette, Isabelle. “The AI Boom is Here. The Cloud May Not Be Ready.” The Wall Street Journal, 10 July 2023.
Caserta, Joe et. al. “The Data Dividend: Fueling Generative AI.” McKinsey & Company, 15 Sept. 2023.
Dilmegani, Cem. “Top Six Challenges of AI in Healthcare and Overcoming Them in 2023.” AIMultiple, 12 June, 2023.
Isaksson, Charlie. “How to Estimate ROI for AI and ML Projects.” phData, 18 Feb. 2022. Accessed 3 Oct. 2023.
National Conference of State Legislatures. ”Artificial Intelligence 2023 Legislation.” NCSL, www.ncsl.org. Accessed 3 Oct. 2023.
Parikh, Ravi B. et al. “Paying for Artificial Intelligence in Medicine.” NPJ Digital Medicine vol. 5, no. 63, 20 May 2022.
Sahni, Nikhil R. et. al. “The Potential Impact of Artificial Intelligence on Healthcare Spending.” NBER Economics of Artificial Intelligence Conference, Jan. 2023.
“The Healthcare Data Explosion.” RBC Capital Markets. www.rbccm.com. Accessed 3 Oct. 2023.
FHIR® is a registered trademark of Health Level Seven (HL7) and is used with the permission of HL7. Use of this trademark does not constitute an endorsement of products/services by HL7®DICOM® is the registered trademark of the National Electrical Manufacturers Association for its Standards publications relating to digital communications of medical information.