Throughout the COVID-19 pandemic, experts have been warning of the dangers of postponed health care services. In January, the American Cancer Society, the National Comprehensive Cancer Network, and 73 other organizations, including many major health care systems, issued a statement stressing the urgency of preventive care. “We urge people across the country to talk with their health care provider to resume regular primary care checkups, recommended cancer screening, and evidence-based cancer treatment (PDF) to lessen the negative impact the pandemic is having on identifying and treating people with cancer,” the groups said.

That was sound advice not everyone could follow, as ProPublica’s Duaa Eldeib reported last week in a tragic story about Teresa Ruvalcaba. The 48-year-old single mother of three worked for 22 years at a candy factory on Chicago’s West Side. During the pandemic, disaster struck. “For more than six months, the 48-year-old factory worker had tried to ignore the pain and inflammation in her chest. She was afraid of visiting a doctor during the pandemic, afraid of missing work, afraid of losing her job, her home, her ability to take care of her three children,” Eldeib reported.
“Even though her chest felt as if it was on fire, she kept working. She didn’t want to get COVID-19 at a doctor’s office or the emergency room, and she was so busy she didn’t have much time to think about her symptoms,” Eldeib wrote.
Ruvalcaba’s pandemic fears were typical of patients across the nation, surveys revealed. A 2020 CHCF poll of 2,249 California adults revealed that even when people wanted to see a doctor for an urgent health problem, one-third did not receive care. Nearly half of those surveyed didn’t receive care for their nonurgent health problems.
Nationally, more than one in three people delayed or skipped care because they were worried about exposure to Covid-19, or because their doctor limited services, according to an Urban Institute analysis of a September 2020 survey.
The toll of this disruption in care — the forgone cancer screening, the chest pain that isn’t reported — will devastate some patients and families. Ruvalcaba had to face a diagnosis with a terrible prognosis, inflammatory breast cancer. “If she would have come six months earlier, it could have been just surgery, chemo and done,” Ruvalcaba’s doctor told Eldeib. “Now she’s incurable.”
Doctors expect the delayed care “could cause worsening health conditions, delayed diagnoses and earlier deaths,” Ana Ibarra reported in CalMatters.
“Unfortunately, we know we’re going to see some tragedies related to the delays,” Wiley Fowler, an oncologist at Dignity Health in Sacramento, told Ibarra.
Consequences of Delayed Care
Public health messages early in the pandemic urged people to avoid public places, including doctor’s offices. In April, as Hayley Smith noted in a Los Angeles Times story, the US Centers for Disease Control and Prevention (CDC) and the Centers for Medicare & Medicaid Services “both published guidelines recommending the postponement of elective and nonurgent procedures, including ‘low-risk cancer’ screenings, amid the first wave of the pandemic.”
Patients and doctors listened. Appointments were canceled. “Nonurgent” procedures encompassing a wide array of treatments and operations, including cancer surgeries, were delayed.
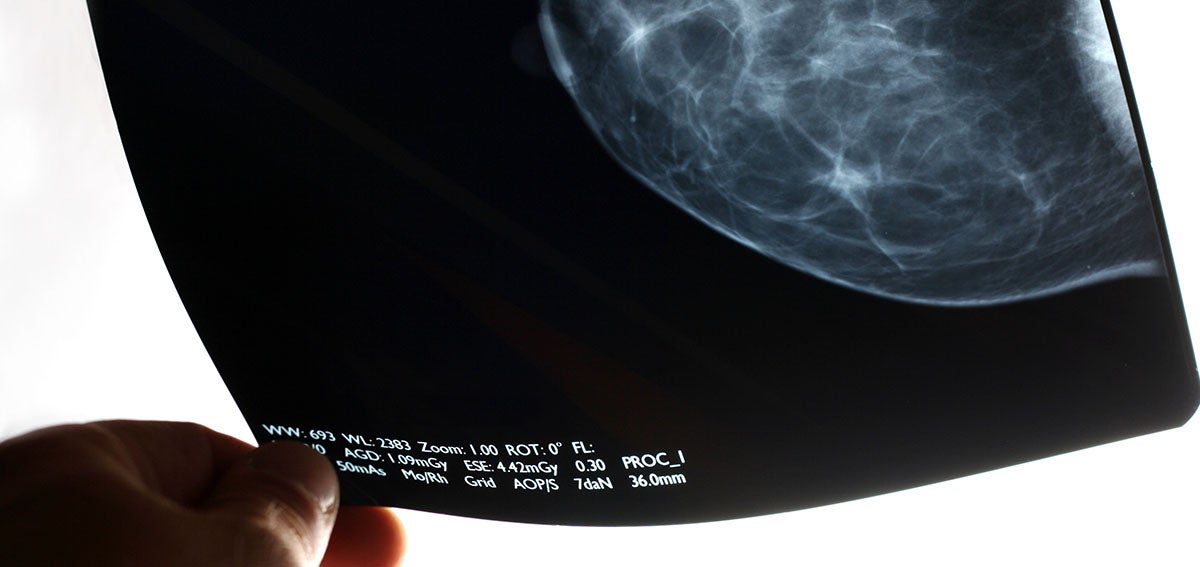
Preventive cancer screenings dropped 94% over the first four months of 2020, Eldeib reported. The National Cancer Institute expects to see 10,000 preventable deaths over the next decade because of pandemic-related delays in diagnosis and treatment of breast and colorectal cancer. Screenings for these cancers, which account for about one in six cancer deaths, are routine features of preventive care.
I know I should get another check soon, but the anxiety of COVID feels like more of a priority than the anxiety of cervical cancer.
—Molly Codner, a Southern Californian who received an abnormal Pap smear last summer
In California, cancer deaths have remained roughly the same as prepandemic rates, but that stability is not expected to last. Based on the National Cancer Institute data, Ibarra calculates that an additional 1,200 Californians will die from breast and colon cancer. The National Cancer Institute estimate is conservative “because it only accounts for a six-month delay in care, and people are postponing care longer than that,” Ibarra reported.
Nationally, death rates from cancer are expected to increase in a year or two. Slow-growing cancers will remain treatable despite a delayed diagnosis, Norman Sharpless, MD, director of the National Cancer Institute, told Eldeib. Yet for conditions like Ruvalcaba’s inflammatory breast cancer, delayed care can be disastrous.
Women, People of Color Disproportionately Affected
For women across Southern California, appointments have been delayed, exams canceled, and screenings postponed during the pandemic, Smith reported in the Los Angeles Times. “Some are voluntarily opting out for fear of encountering the virus,” Smith wrote, “while others have had their appointments canceled by health care providers rerouting resources to COVID-19 patients.”
Before Pap smears became part of routine American health care, cervical cancer was one of the deadliest cancers for women. Today, as many as 93% of cervical cancer cases are preventable, according to the CDC, and screenings are a crucial component of preventive care. Yet during the first phase of California’s stay-at-home orders, cervical cancer screenings dropped 80% among the 1.5 million women in Kaiser Permanente’s regional network, Smith wrote.
The effects of the pandemic shutdown extended beyond delayed Pap smears. Women who spoke to Smith said that “mammograms, fertility treatments and even pain prevention procedures have been waylaid by the pandemic.”
Sometimes, obstacles other than the pandemic are continuing to interfere with access to care. One woman had an appointment delayed and then lost her job and her health insurance, Smith reported.
“Molly Codner, 30, has needed a checkup ever since she received an abnormal Pap smear last summer,” Smith wrote, “but like many Southern Californians, the trauma of the last year still weighs heavily on her mind: Nearly a dozen people she knows have had COVID-19.” Codner told Smith that “I know I should get another check soon, but the anxiety of COVID feels like more of a priority than the anxiety of cervical cancer.”
People who face disparities in treatment and care are most likely to be hard hit by pandemic delays. That includes Black people, who were already more likely to die from cancer than any other racial group. Cancer also is the leading cause of death among Latinx people. Breast cancer is the most common cancer diagnosis for Latinx women. Overall, more Americans die of heart disease.
Black adults are more likely than White or Latinx adults to delay or forgo care, according to researchers from the Urban Institute.
Telehealth Solved Access Issues for Some, Not All
Telehealth was a boon for patients during the pandemic year. Yet, as Ibarra notes, “there’s only so much that doctors and nurses can do through a screen.” Dental visits, mammograms, and annual wellness checks were also put on hold by the pandemic.
Unequal access is another challenge for telehealth. The benefits of the telehealth boom were not shared equally, according to a statewide survey conducted last month by the University of Southern California and the California Emerging Technology Fund.
Latinx, Asian, and Black respondents did not use telehealth as often as White respondents. USC researchers attribute these differences to “disparities in income, education and access to any kind of health care.”
Researchers at the Urban Institute report similar findings: “Black and Latinx adults were more likely than White adults to report having wanted a telehealth visit but not receiving one since the pandemic began, and that difficulties getting a telehealth visit were also more common among adults who were in poorer health or had chronic health conditions.”
After controlling for socioeconomic factors and health status, patients with limited English were half as likely to use telehealth compared to fluent English-speaking patients, the Urban Institute said. “Much work remains to ensure all patients have equitable access to remote care during and after the pandemic,” the researchers wrote.
Whether telehealth is conducted by video or phone may be crucial to ensuring access to care. A study of telehealth use at Federally Qualified Health Centers in California in 2020 found that “more primary care visits among health centers in the study occurred via audio-only visits (49%) than in-person (48%) or via video (3%). Audio-only visits comprised more than 90% of all telemedicine visits.”
“For many Californians with low incomes, the ability to connect with a doctor or their care team by phone or video is much more than a convenience,” Chris Perrone, director of CHCF’s Improving Access team, explained on The CHCF Blog. “It’s really the difference between canceling a visit because the barriers are too great or getting the timely care that they or their child needs.”
Pandemic Health Effects Will Outlast COVID-19
Public health efforts might need to focus on two goals at the same time as the US recovers from the pandemic: increasing vaccine uptake to keep COVID-19 in check and proactively managing the fallout from delayed care.
“As we focus on recovery, we have to ensure that we get vaccinated,” Efrain Talamantes, a primary care physician in East Los Angeles, told Ibarra. “But also that we have a concerted effort to manage the chronic diseases that haven’t received the attention required to avoid complications.”


