The previous article in this series introduced the topic of generative AI in the back office of healthcare. This article starts to look at healthcare generative AI use cases.
Is it any surprise that new technologies in health care pop up quickly in the area of reimbursements? Payments are the constant obsession of every manager.
Claims
Abhishek Sharma, principal of business transformation at Sagility, says that payers question why a doctor ordered an MRI instead of a less costly CT scan, and that precise details in the patient’s medical record and clinical demographic history have to be culled to justify the decision.
Dushyant Mishra, co-founder and CEO of RapidClaims, says that five to ten percent of costs in clinical institutions goes to billing and revenue management. The international ICD classification of diseases and conditions went from about 13,000 codes in ICD-9 to 68,000 in ICD-10. ICD-11 has already been formalized but is not in widespread use.
It’s really too much to expect a human coder to find the most appropriate code (translate: the code most likely to maximize reimbursement). Doing so requires checking historical records for symptoms, test results, and other data that the payer needs to validate a code.
Moreover, codes are routinely being added and deleted, and payers change their criteria for approving them. Mishra says that payers handle codes differently, some separating conditions and others preferring them to be combined. Ongoing training is required for human coders. It’s a textbook use case for AI.
Anna Twomey, senior director of healthcare at SS&C Blue Prism, lays out examples of subtleties that a human coder might miss. Sometimes, for instance, multiple medication pills are billed as a single dose. She says, “Additionally, the decision between bundled and unbundled procedures has significant impacts on billing. Human analysts may not always have the time to verify if all steps in a bundled procedure are accounted for, potentially missing charges. Generative AI, especially when combined with Robotic Process Automation (RPA), can meticulously analyze these procedures to ensure all relevant charges are identified and billed appropriately. In one organization, generative AI recovered more than a million dollars in missed (unbilled) dollars in a single quarter.”
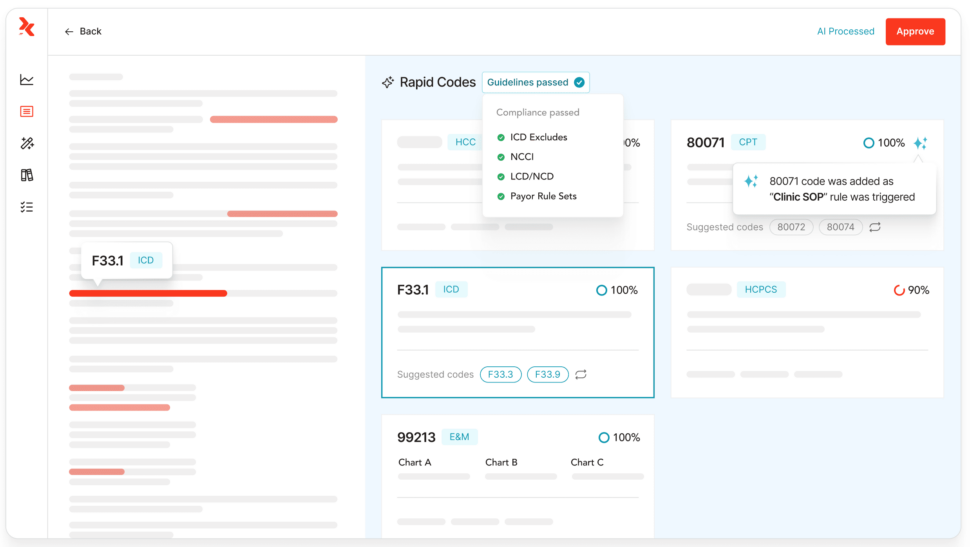
RapidClaims, which just announced a major funding round, focuses on automated medical coding. Mishra says that it doesn’t require a change to coders’ workflows. The efficiency provided by RapidClaims allows clinicians to increase the number of charts they process by 100% or more, leading to faster reimbursements. Figure 1 shows a RapidClaims dashboard.
My experience suggests that faster billing produces benefits for patients, too. How often have you received a surprise bill asking you to pay for some test or procedure that took place so long ago, you’ve forgotten it?
RapidClaims is focusing now on ICD-11 and thinks that their service will make the transition much easier for clinicians.
Akshay Sharma, chief AI officer at Lyric, describes rules for billing as a complicated set of layers of policies, with the Centers for Medicare & Medicaid Services (CMS), states, and private payers issuing large collections of clinical policy documents on a regular basis as new medications, diseases, and symptoms emerge. Thousands of pages of policies need to be evaluated as often as once a month.
“We’re capable of revealing the true impact of changes in documents longitudinally,” he writes. This approach, referred to as “reasoning based on unstructured text using language models,” uncovers specific extracts within the documents. These extracts are then presented to a human expert, who can offer feedback to help shape policies.
I suggested to him that it would make sense for the regulators to produce their own summaries, and he said he would like that to happen, but that they have no incentive to do so.
Lyric’s AI, based on a large corpus of knowledge built over decades, can also explain the adjudication decisions that have been made. Sharma writes, “The AI-based outputs are reviewed by experts who can provide feedback, which helps us improve the models. Specialized knowledge packs are built for payers to deploy the accurate setup.”
They also have plans to use generative AI for code generation. Sharma says, “This technology will assist in generating test cases and base code, ultimately enhancing the time to market for continually evolving policies.”
Iodine Software, according to Priti Shah, chief product and technology officer, uses AI to streamline utilization review in support of case management and documenting medical necessity, resulting in reduced insurance claims denials.
Prior Authorizations and Appeals
Next to billing, prior authorizations and appeals take up much of administrators’ attention. Doug Ross is vice president, US head of generative AI at Sogeti, part of Capgemini. He says the inputs to a prior authorization request vary for each type, and that generative AI can check whether all the necessary inputs are present in the request.
Experian Health released their AI Advantage program during the past year, aimed at large providers and offering various support for revenue cycle management. According to Clarissa Riggins, their chief product officer, one of their services is denial triage: deciding which denials have the highest chance of a successful appeal.
Riggins says that getting approvals is not straightforward, but depends on a knowledge of how a particular payer will react, a “tribal knowledge” that staff learn over time. She says there are a lot of “if…then…else” decisions that generative AI can help you make. Such complexities arise when a patient has multiple insurance plans, or other sources of funding such as a charity.
Abhishek Sharma also describes how Sagility helps providers harness Generative AI to generate customized appeal letters, by summarizing requisite data points from a medical record. Conversely, Sagility aids payers by employing LLM-based classifiers for more precise identification and prioritization of incoming appeals, enabling the assignment of an expedited or urgent status when warranted.
Resource Management
Seek AI, according to founder and CEO Sarah Nagy, provides a natural language processing (NLP) interface that lets staff pose a wide range of questions with immediate responses, such as “How many patients did we see this week in comparison to last week?” Figure 2 shows a typical report from Seek AI.
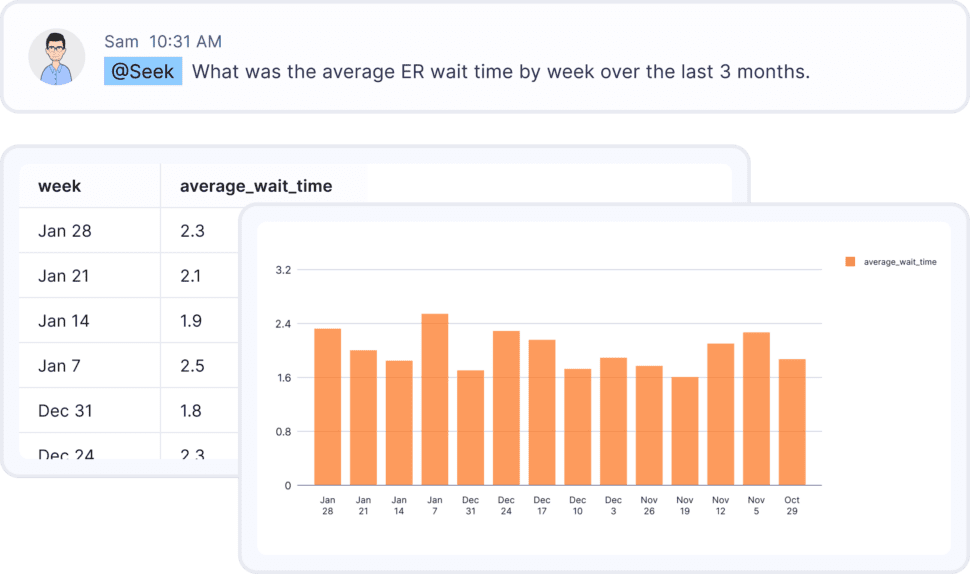
Nagy claims that Seek AI’s model is the world’s most accurate for typed language recognition for data.
Contract Generation
HSBlox provides a Value-Based Care Administration (VBCA) Platform that includes contract modeling and a contract builder. CEO Rahul Sharma explained to me that the platform has the flexibility to extract the pertinent data by processing existing contracts or digitization of traditional datasets. The company is building an interim stage in this process using generative AI. By training large language models (LLMs) on past contracts, generative AI can generate new contracts based on past patterns that can then be reviewed and finalized.
The platform passes that input through several stages. First, the contract modeler uses a combination of a rules-based engine and a query builder, built on Microsoft’s Power BI. Sensitivity analysis is performed by changing input variables, which determine the outcome of a decision given the combination of certain ranges and values of variables such as prices, coverage, and expiration dates. LLMs can analyze individual components of complex and lengthy contracts to extract those specific values.
Once the contract has been modeled, end users can use information from the contract modeler to build out the contract for different use cases. End users can also clone an existing contract from the library to edit and save as a new contract, based on sensitivity analysis done during the contract modeling stage. Sharma says, “This information can be extracted within seconds and presented with a simple-to-use workflow that allows users to finalize contracts within days.”
He emphasized that they are using a “data privacy vault” based on the IEEE’s recommended architecture for securely storing, managing, and using patient information by de-identifying fields. The de-identified data can safely be submitted to an LLM.
The next article continues to look at interesting uses for generative AI in the back office of healthcare.













