While people in the U.S. perceive a dramatic rise in mental health conditions among fellow health citizens growing over the past five years, people note barriers of cost, insufficient supply of providers, and stigma as barriers to getting care in the latest Gallup and West Health poll on the subject. 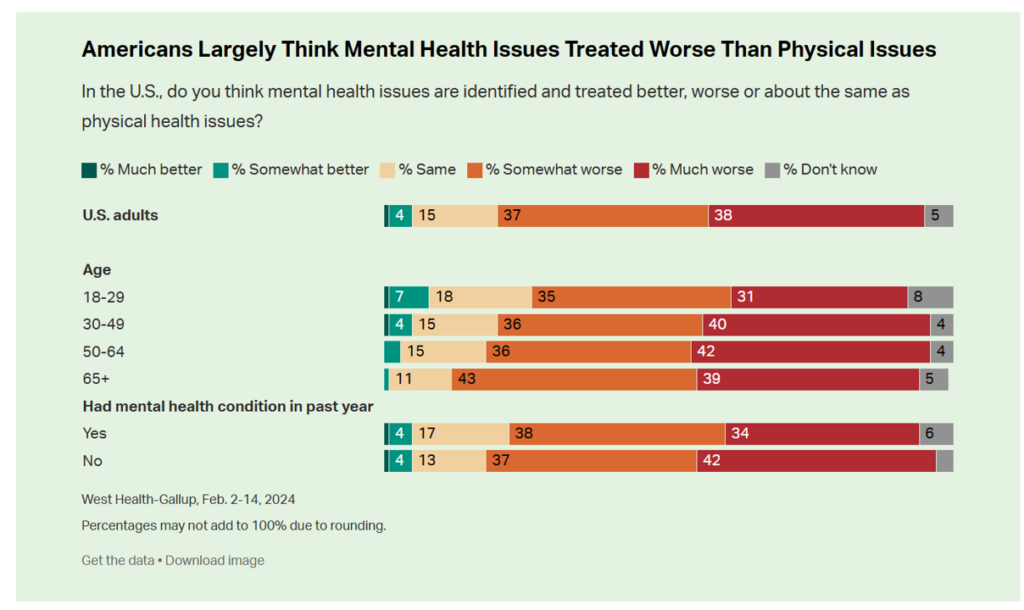
In West Health’s words, three-quarters of Americans feel that, “mental health takes a back seat to physical health” in the U.S.
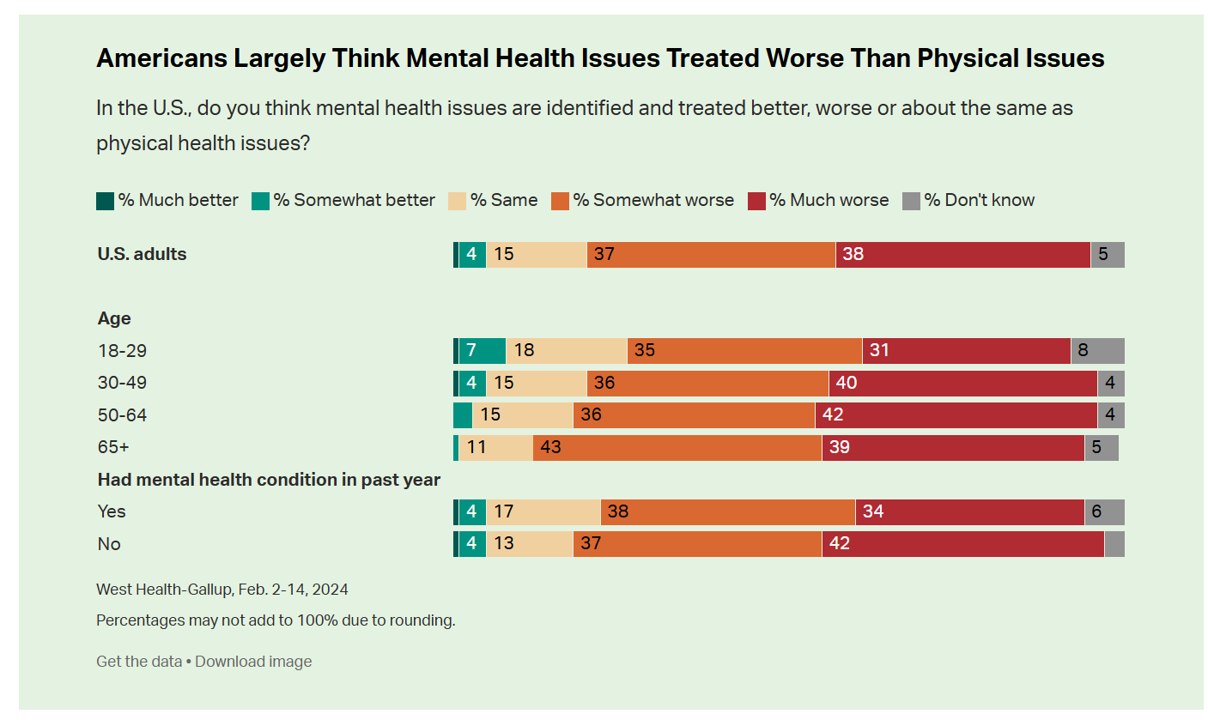
A key theme of the research found that Americans find that mental health is not treated as well as physical health in the U.S.: the first bar chart tells us that only about 5% of people see mental health issues “identified and treated better” than physical health issues.
Quite the opposite, 3 in 4 Americans say mental health is treated worse.
And one-half of people in this study said they had experienced depression, anxiety, or another mental or emotional condition in the past 12 months.
Gallup and West Health conducted the study in early February 2024 among 2,266 U.S. adults 18 and older.

May is Mental Health Awareness Month each year, so time to be even more vigilant in calling out the Gallup findings and continued stigma and barriers to accessing needed services. In social media you can follow #MHAM2024 and check out the SAMHSA website for a comprehensive toolkit to support your own efforts in bolstering awareness of this public health epidemic in the U.S.
In the meantime, more older people feel the mental/physical health service gap even more acutely than younger health citizens. And it’s important to call out that older people typically deal with more chronic (physical) health conditions than younger people do, so the lack of integrating mental with physical health services (especially in primary care) is concerning.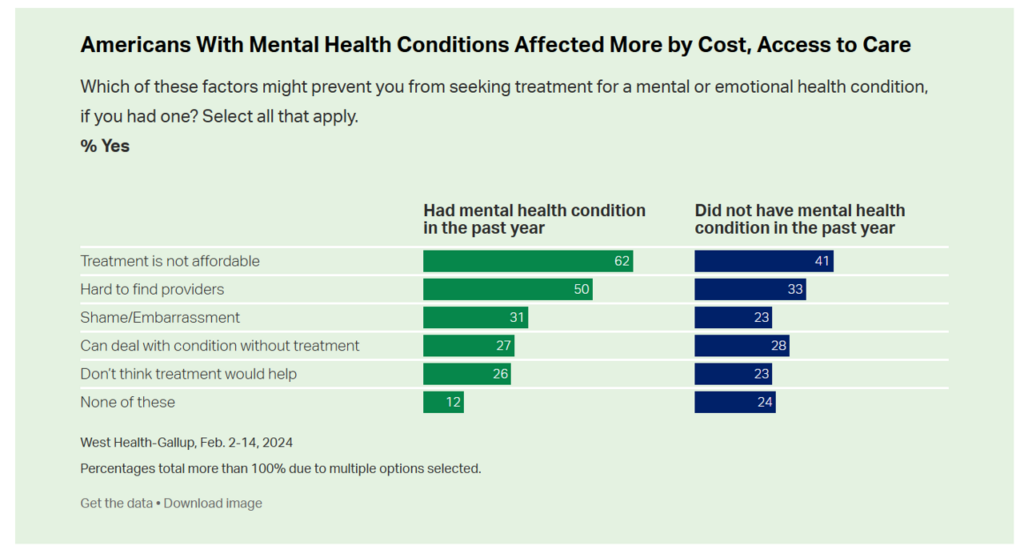
This chart illustrates that people dealing with a mental health condition were more negatively impacted by cost of the mental health services, challenges with finding a provider in their community (the supply side challenge), and taboo or shame about seeking such care: that is,
- Treatment not affordable noted by 62% of Americans with a mental health condition in the past year (vs. 41% who did not have a mental health issue)
- 50% of people dealing with mental health problems finding it hard to find a provider, vs. 33% of folks who did not have a mental health condition, and,
- 31% of people who faced shame or embarrassment (taboo) with a mental health issue compared with 23% of people who did not.

Health Populi’s Hot Points: Only 1% of Americans gave the U.S. health care system an “A” for mental health services, with 8% of people in the U.S. grading mental health a “B.” The average grade is heavily weighted toward D-F with 57% of people granting one of these two grades for mental health care in America.
It’s important to note that most of those polled believe that counseling or therapy would be more effective than medication for mental health.
And telehealth has played an important role to fill in the long-time gap in the supply side of therapists for Americans long without a source of mental health care for counseling or talk therapy.
According to the latest FAIR Health data, it’s telemental health that has had to greatest continued up-take among U.S. consumers, both older and younger, to access mental health services more than physical health encounters with either PCPs or specialists of all types. 
One provider of tele-mental health services had been Walmart, whose price list is shown here for a variety of Walmart Health brick-and-mortar clinic and virtual care services.
This list is an historical artifact now with Walmart’s announcing on 30th April its exit from Walmart Health‘s clinics and virtual care platforms.
The fact that Walmart Health offered counseling services for basically $1 a minute for talk-therapy — $60 (for an hour) of new patient intake encounters, and $45 for individual counseling (for 45 minutes) — brought access to people who had lacked value-based access to therapy. That is, value in the eye of the patient-consumer.
The market exits of other telehealth providers is part of a larger retrenchment of virtual care. This also blurs with a challenging primary care environment long under-funded in the U.S. compared with other OECD/developed nations whose health outcomes far surpass those of America’s, and whose on-ramps to primary care are assured and universal for their nation’s health citizens.
Mental health is physical health, and telehealth is health and health care. So it behooves us to watch and listen to coverage of next week’s ATA Nexus meeting updates to stay up-to-speed on the many facets to our challenge — for the very short-term assurance of providing care to people who need it — and longer-term, how the public and private sectors can collaborate to assure parity of mental and physical care for all — with mental health care bundled into primary care from the jump.




 Thanks to Feedspot for identifying
Thanks to Feedspot for identifying  Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.