This post follows up Part 1 of a two-part series I’ve prepared in advance of the AHIP 2024 conference where I’ll be brainstorming these scenarios with a panel of folks who know their stuff in technology, health care and hospital systems, retail health, and pharmacy, among other key issues.
Now, let’s dive into the four alternative futures built off of our two driving forces we discussed in Part 1.
![]()
The stories: 4 future health care worlds for 2030
My goal for this post and for the AHIP panel is to brainstorm what the person’s health care experience would be in each of these four worlds.
The four stories we generate are:
- Retail Health For All, starring “The Consumer”
- DIY Healthcare, starring “The CEO”
- Fragmentation Meets Bureaucracy, starring “The Castaway,” and,
- “One World, One Health,” starring “The Health Citizen.”
A caveat: I do this exercise with clients over the course of an intense immersive weekend or over many weeks (convening weekly or biweekly meetings). This is your bite-sized version, which I’ve created as a “thinker-toy” for you to consider in your planning efforts….looking far enough in the future from now to 2030, recognizing that we will have had two U.S. Presidential elections to that point, and that the last retiring Baby Boomer enrolls in Medicare that year.
Let’s take a walk with “Quincy” through each of the four worlds to see how their health care experience might play out across the key driving forces.
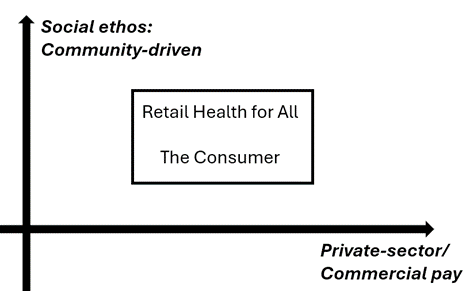
Retail Health for All, starring The Consumer
- Social ethos – community-driven
- HC financing – private-sector/commercial
U.S. health care in 2030 is based on Retail Health for All, with a community-focused orientation financed largely through the private sector and commercial payment – including some level of self-pay by The Consumer, who plays the starring role in this health care world.
Health care is delivered through an omnichannel platform accessible to all consumers, tailored for personalization. Quincy has great trust in this health care system, appreciating that customization also takes into account peoples’ values, ethnicities, and clinical needs. Clinicians partner with patients, often in teams and group-based care.
AI informs personalization to the N of 1, and Quincy takes advantage of consumer technology available through his favorite retailer for self-care at home. Their home is the site for most of their health care, with sensors in the kitchen, bedroom, bathroom, and in the car all informing Quincy’s digital phenotype that further populates data into their EHR which they control and audit.
Quincy also values that in a community-based system for care, national standards have been adopted for care and protocols, further bolstering health equity in their community and workplace. Their employer pays for a level of care and services above which Quincy spends additional funds for services they value. Quincy’s community appreciates that everyone has access to primary and tertiary care, most of which starts with virtual services delivered at home or work or on-the-go. Telehealth happens across the U.S. as clinicians do not face issues of State licensure barriers. The community accepts some cost-tiering based on personal preferences.
Due to the collective ethos in the community, gun safety has been addressed as a public health issue, and the health care system and employers are committed to assuring cybersecurity and the protection of individuals’ health data. Privacy laws have evolved on a national basis that have used the Washington State Privacy Law, the My Health My Data Act of 2023.
There has been merger and acquisition activity among providers consolidating regional systems, with some private equity activity that has carefully regulated to ensure The Consumer’s rights are protected. Quincy trusts the many touchpoints in their health care – the government not so much as payer or plan sponsor but as standards-setter and convener to ensure safety, security, and environmental health on a national basis for all Consumers.
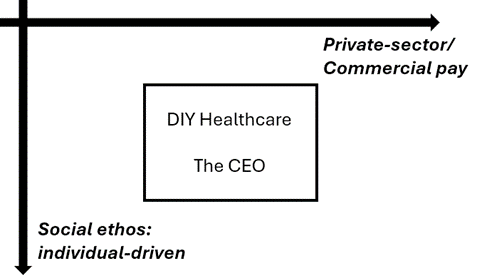
DIY Healthcare, starring The CEO
- Social ethos – individualistic
- HC financing – private-sector/commercial
The person is The CEO of their own health care in 2030: Quincy values the personalization they benefit from in DIY Healthcare, deriving much of their care through Big Retail and Big Tech providers who manage teams of clinicians in digital-first workflows.
In this more individualistic health care landscape, Quincy can take advantage of niche-delivered services in the community and at home, paid-for by employers and private sector organizations, AI informs personalization and self-managed coaching through apps and digital tech delivered in an a la carte mode,
Loneliness remains a challenge for many people in the DIY Healthcare mode, with mental health services delivered via virtual tech platforms which endeavor to incorporate design elements that mimic “belongingness.”
There is more PE-backed innovation for smaller niched digital tech companies that deliver services to The CEOs of health care-self-care, and more out of pocket spending by Quincy and their friends and family base don personal preferences.
Based on more isolated lifestyles, Quincy and friends used many forms of sensors in their homes, especially for PERS systems, safety, and security. There are more cyber-threats and risks in DIY Healthcare given more fragmentation and niche-products, and less collaboration across the ecosystem.
State license is also more fragmented with wealthier consumers gaining access to services who are willing to pay more out of pocket. Concierge care thrives for those who can afford to take advantage of it.
Trust lies closer to home, with the people I know, and my employer. Science is trusted especially when it fits my paradigm for self-care and how I define the “CEO of me.”
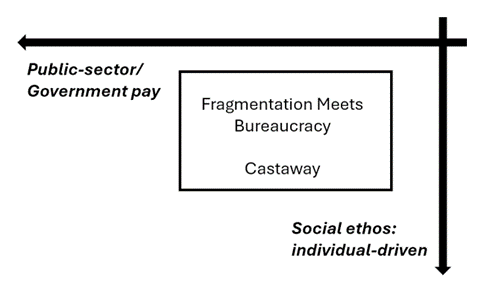
Fragmentation Meets Bureaucracy, starring The Castaway
- Social ethos – individualistic, high
- HC financing – public sector/government
The fragmented U.S. health care system challenges Quincy who feels isolated and dis-empowered when it comes to their care – both in terms of accessing services and their personal health information, which is difficult to get. Disparities and techquity gaps persist in 2030 in this heavily-bureaucratized health care world, which is under-funded by the public sector.
There are also significant variations in care and outcomes based on the State in which people live: Quincy’s State is more affluent in terms of tax-base and health care capital resources, compared with his cousin living in a nearby State which has a long history of poor public health, lack of good education for residents, and high levels of smoking and substance use.
Only the best-resourced hospitals are able to access innovations. There are drug shortages and service queues in some regions where patients feel like castaways in health care deserts.
Trust is in short supply for all institutions, not just government: even the health system lacks the public’s trust who feel betrayed by having to wait for care, self-ration services and medicines due to cost, and still bear medical debt when faced with high-cost services not covered by the public payers.
The lack of social cohesion exacerbates Quincy’s and other’s mental health, ticking up the level of Deaths of Despair that had somewhat resolved in the latter 2020s.
The public sector bureaucracy overwhelms the lack of investment in a cohesive information system that patients like Quincy can access. Add to this Quincy’s patient administrative burden of paperwork and navigation having to spend much more time than his cousin in Massachusetts which has ensured patients’ access to their health information via portal.
The lack of continuity of care due to fragmentation adds to the cost of care in this health care world. Furthermore, the individualistic social ethos supports social media-proliferated conspiracy theories and mistrust in science and health experts. Fueling this scenario is a society and polity that has not dealt with gun safety, which remains a challenge in this health care world that de-values community, public health, and environmental safety.
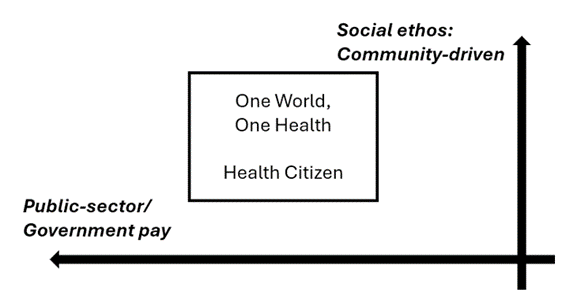
One World, One Health, starring the Health Citizen
- Social ethos – community-driven
- HC financing – public sector/government
Living as a Health Citizen in the One World, One Health health care environment, Quincy enjoys and values a level of health security that is similar to health citizens living in parts of Europe, in Japan and Australia/New Zealand. Quincy, family and friends take on good health behaviors that create a flywheel virtuous cycle of others’ behaving well, with low levels of smoking, binge drinking, and other negative lifestyles.
Health equity is prioritized in Quincy’s community as a community investment. Team-based care is delivered for all health citizens, starting with primary care “in every pot.” Virtual and telehealth services are available to all, everyone connected to ubiquitous broadband which is provided as a public utility.
The public sector has invested in a unified EHR (Epic for All) with full data interoperability and citizen access/control of data. Privacy protections are assured through the GDPR which the U.S. adopted based on Europe’s implementation of that privacy directive.
Innovation happens at-scale as clinical trials and other pathways to research and development are viewed as national assets. The community ethos bolsters social cohesion and mental health.
Thus, there is a national/Federal approach to health care adopting protocols and reducing variation. Health citizens value this national approach, with health baked in all public policies. As taxpayers’ willingness to trade off higher taxes for benefits for all. Fewer employers feel compelled to provide health insurance in this environment.
Federal gun legislation is passed and investments in cybersecurity are maxed in this scenario, with policies and procedures in the workplace taken seriously by all health citizens.
Federal investment in climate and environmental health are part of holistic health policy. Local communities support, and are supported, for clean air and water, and local construction codes support healthy buildings and walkability in town planning.
There is a careful balance between M&A and consolidation with respect to antitrust: combined organizations must provide community benefit to trade-off market concentration. There is no distinction for state licensure with respect to telehealth regulations. Regional centers of excellence naturally go national.
Trust is the key currency of health citizenship: earned by organizations and rewarded by ciizens’ loyalty. Transparency reigns and is key to making this work, and citizens take advantage of available information to make informed decisions and share their experiences with others in peer-to-peer health networks. Mis- and dis-information is quickly rooted out and discouraged as anti-social behavior in the One-World, One-Health system,
Consider the Wild Cards
Now that you have lived a few minutes in each of the four 2030 health care worlds, it’s useful to consider Wild Cards: these are low probability events that, if they occur, dramatically change the futures and play out in different ways.
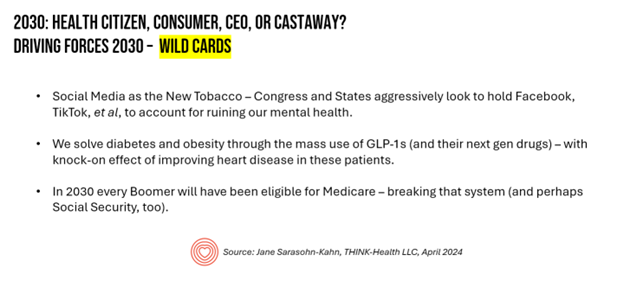
In 2030, I imagine three Wild Cards – only limited by your imagination when you undertake scenario planning. For 2030, consider….
Social Media is the New Tobacco. Thanks to Ian Morrison’s input into my early thinking through these scenarios, he offered up this Wild Card which asks us to wonder what would happen if Congress and the States aggressively look to hold Facebook, TikTok, et al., to account for ruining our mental health.
We solve the syndemic of Obesity, Type 2 Diabetes, and Heart Disease with the mass adoption of GLP-1 meds (and their future counterparts). Imagine if the U.S. health system could excise $1 trillion from national health spending by realizing this Wild Card.
In 2030, every Boomer will have been eligible for Medicare. Then Medicare goes bust. What then? This Wild Card may not be so wild, but it’s certainly worth dealing into our deck of the un-thinkables.
What Next? Stress-Test Your Strategy
You have four alternative worlds to consider for 2030, some six years from “now.”
How would these different futures play with your current strategy?
This is the opportunity to stress-test what’s in your plans and your mind-set. Consider the Wild Cards. Re-visit the list of driving forces to sort out which of these are most germane to your own business or product or marketspace.
At any point in time, we will each be or feel like a Consumer shopping for care, a CEO empowered in our care, a Castaway in the midst of a care journey, or a Health Citizen fully-embracing our rights and responsibilities for care in our community.
I’ve not provided this content to preach or promote one world over another – rather, to help you kickstart some thinking about the future, which is often a daunting prospect especially in light of the many uncertainties all of us face. Let’s face them together, with facts and at the same time, embracing and risk-managing the uncertainties.
And as “Quincy,” in the form of John Quincy Adams, might counsel us –
“If your actions inspire others to dream more, learn more, do more, and become more, you are a leader.”




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.