What’s Behind the Medicare Slowdown?
Digital Health Wire
SEPTEMBER 6, 2023
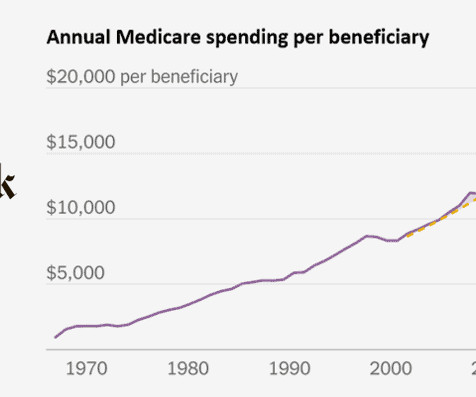
Since Medicare coverage first took effect almost six decades ago, the program’s runaway spending has played a leading role in the story of the federal budget. An excellent piece in The New York Times highlighted how Medicare’s unsustainable climb reached a turning point in 2011, and for reasons that aren’t exactly clear.






































Let's personalize your content