We are only just past the dawn of the second machine age, where digitization is enabling artificial intelligence. “Our new tools are destroying both trust and truth, creating a hunger for community and authenticity. We crave actual physical connection to neighbours, colleagues, and fellow townspeople, even if digitally facilitated.”
Anne-Marie Slaughter wrote this in a column I read this morning in the Financial Times titled, “Our struggle with technology to protect trust and truth.”
Trust and truth underpin health engagement, we learned in the first Edelman Health Engagement Barometer launched ten years ago. Those were the early days of the formation of patient social networks [Patients Like me was founded in 2004, and WEGO Health and Stupid Cancer in 2007]. Those communities have matured and a decade later, led to the New England Journal of Medicine‘s Catalyst community assessing how social networks can improve patient health. The Insights Report from this study is available here.
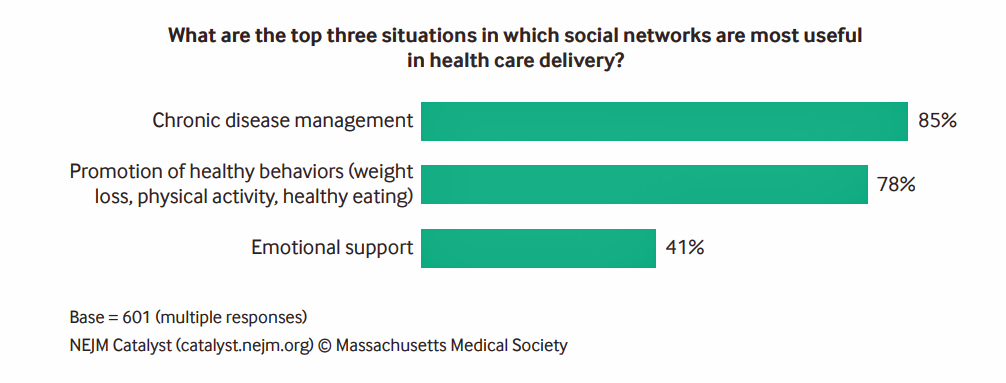
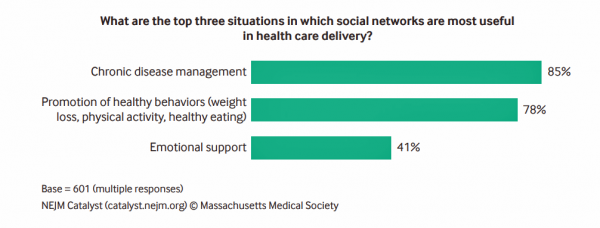
Social networks are useful in health care delivery, virtually all healthcare stakeholders agreed. The biggest opportunities from the Council’s point of view are for managing chronic diseases and promoting healthy behaviors, followed by providing a platform for emotional support.
For context in interpreting these findings, note that the Catalyst panel is comprised of health care executives, clinical leaders and clinicians — with no patient or consumer input.
 “Awareness is growing that social networks in health care…can help people improve health behaviors. Peer networks can provide information and community to patients who otherwise might struggle alone with a new or existing disease,” Dr. Kevin Volpp of University of Pennsylvania and Dr. Namita Mohta of Brigham and Women’s Hospital co-write in the report.
“Awareness is growing that social networks in health care…can help people improve health behaviors. Peer networks can provide information and community to patients who otherwise might struggle alone with a new or existing disease,” Dr. Kevin Volpp of University of Pennsylvania and Dr. Namita Mohta of Brigham and Women’s Hospital co-write in the report.
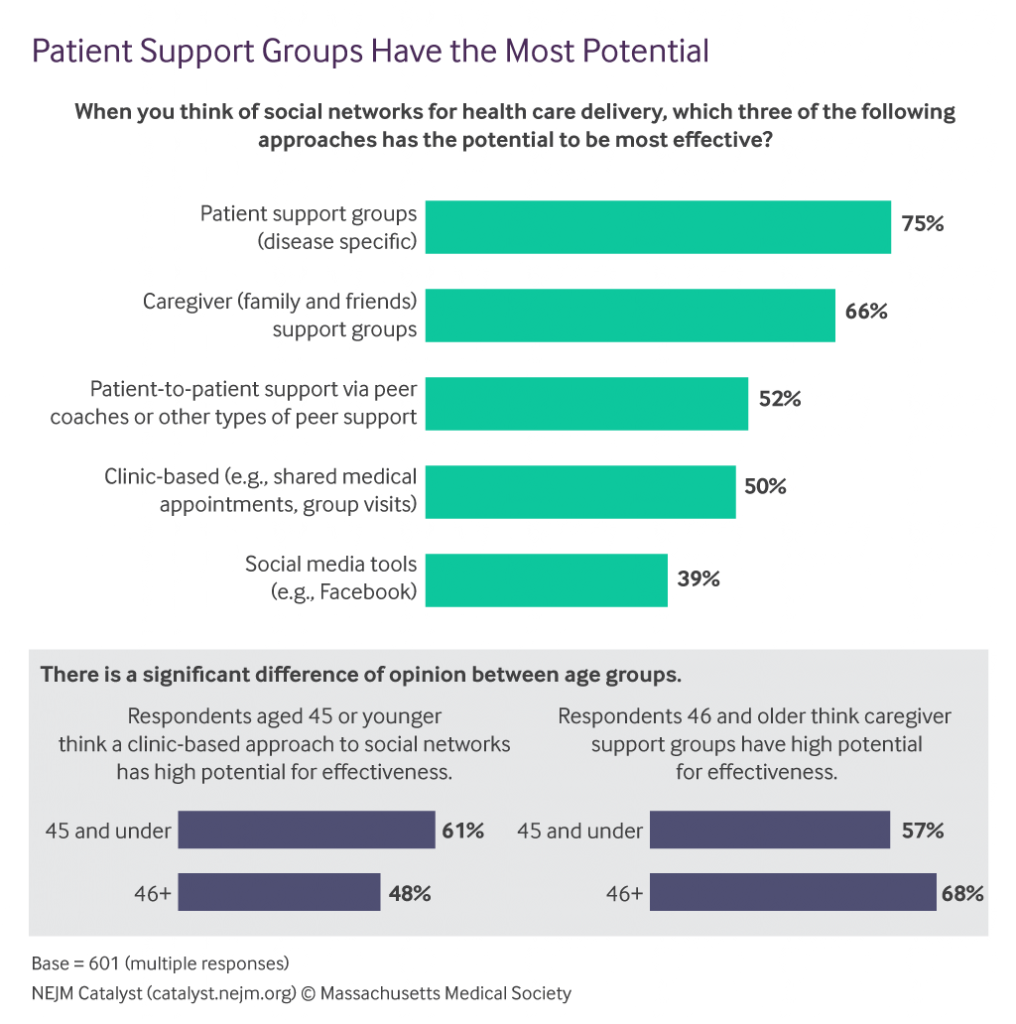
What’s driving health care providers to tap into social networks, Volpp and Mohta believe, is the growing financial risk assumed by health systems. Social networks give providers-at-risk the opportunity to scale care to larger patient populations, identifying disease-specific patient support groups and caregiver support groups as very powerful platforms for that scaling.
One practical benefit of patient social communities is that they may be a more “stable channel” for connecting with patients, given that consumers often switch cell numbers versus changing their social media identities on, say, Facebook.
Two-thirds of healthcare providers prefer face-to-face group sessions as the top choice for communication — that is, in-person social networks — versus 50% who say social media sites (like Facebook) are most useful for communication. One-half of providers also believe that face-to-face, one-on-one sessions with social network members are most useful for communicating.
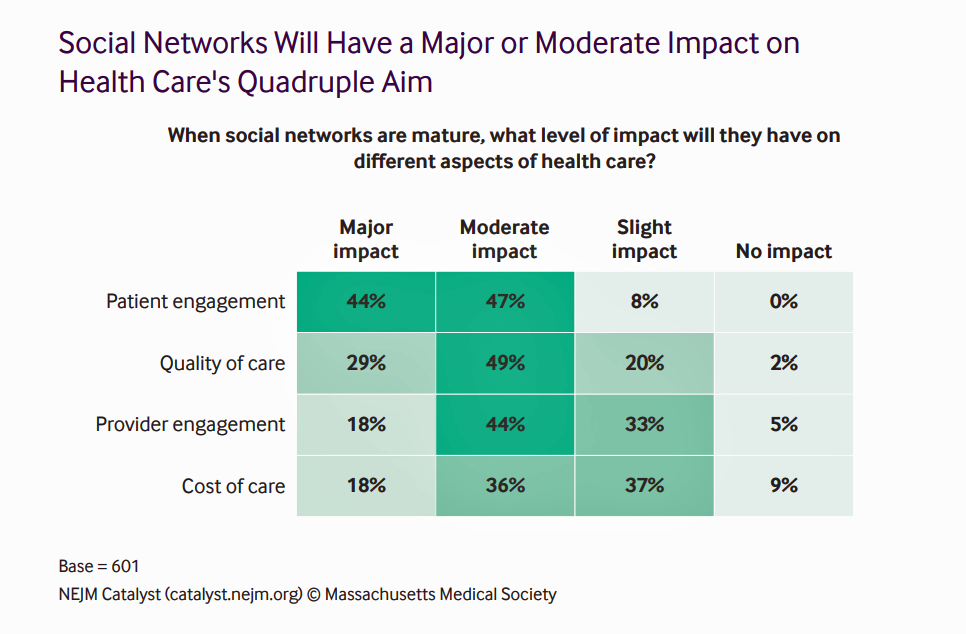 How impactful might social networks be on different aspects of health care? The biggest impacts, Catalyst members say, will be on patient engagement, quality of care, and provider engagement. Over one-half of providers believe social networks, once mature, would also impact the cost of care in a moderate or major way.
How impactful might social networks be on different aspects of health care? The biggest impacts, Catalyst members say, will be on patient engagement, quality of care, and provider engagement. Over one-half of providers believe social networks, once mature, would also impact the cost of care in a moderate or major way.
Health Populi’s Hot Points: Jack Barrette, CEO and Founder of WEGO Health, published a paper earlier this month on the impact of Facebook’s news feed changes on patient social networks.
Having analyzed the new Facebook approach, his bottom line is: “Leverage the truly authentic voice of the patient. User-generated content that features trusted Patient Influencers and their real stories will likely increase Facebook engagement rates and be prioritized in audience news feeds.”
So we return to Anne-Marie Slaughter’s final insight, three paragraphs from the conclusion of her column: that recovering a belief in truth might happen through direct engagement with “purveyors of news and stories, through the creation, ironically, of Facebook groups.”




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.