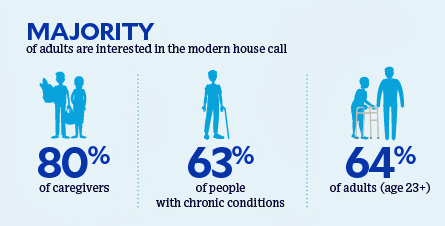
 Most people dealing with chronic conditions, and those who care for them, believe that “home is where the health is,” according to a survey about the “21st century house call” from CareMore Health.
Most people dealing with chronic conditions, and those who care for them, believe that “home is where the health is,” according to a survey about the “21st century house call” from CareMore Health.
To gain peoples’ perspectives on health care at home and chronic disease management, CareMore Health and Aspire Health commissioned a survey among 2,009 U.S. adults 23 years of age and over in September and October 2019. The survey sample included people dealing with chronic disease themselves, as well as caregivers attending to people with chronic illnesses.
The definition of that “modern house call” is largely based on the model of care delivered by CareMore Health — a team-based approach that serves the whole person beyond their diagnosis.
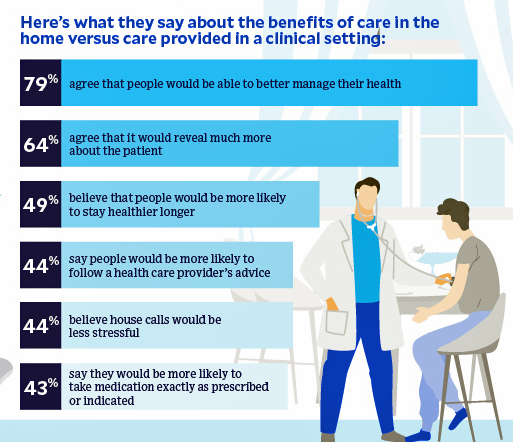
Most consumers identify two key benefits of receiving health care at home compared with a clinical setting like a doctor’s office or clinic: first, that people could better able manage their health in their homes and second, that providers entering the patient’s home for care would learn more about the patient in his/her “native setting” — for example, noting safe living environments, food in the fridge, and working electricity among other social determinants that reach beyond the traditional electronic health record medical history.
One-half of consumers also believe people would be more likely to be healthier longer with care delivered at home, and nearly half of people also think people could be more adherent to medical advice and less stressed in the process.
Most caregivers studied also said the new model of a house call could help overcome challenges their loved one faces in getting to the doctor, as well as helping to share the care responsibility when dealing with their own daily lives, family and work responsibilities.
 Health Populi’s Hot Points: Nearly 9 in 10 people polled said they wanted their health care providers to treat them like a member of their family.
Health Populi’s Hot Points: Nearly 9 in 10 people polled said they wanted their health care providers to treat them like a member of their family.
This photo and text come from CareMore Health’s website, which speaks to the familial touch via “Care you would give your family.”
Further on CareMore Health’s “about” page, you’ll read that, “A disease’s impact isn’t limited to its symptoms—it can affect daily routines, habits, and social connections. That’s why we do not focus solely on treating health issues but aim to solve the root cause, whether it is health, behavioral, economic, or social. Every one of our care centers is filled with stories of CareMore clinicians going above and beyond for their patients.”
CareMore Health has been gathering evidence of patient outcomes delivered through its model of care delivery and larger focus on the whole person vs. a patient’s condition. For example, the organization’s Togetherness Program targeted the loneliness that can be part of older people aging at home; through social workers’ and volunteers’ outreach by telephone and in-person visits, CareMore members had lower emergency room utilization and fewer hospital admissions.
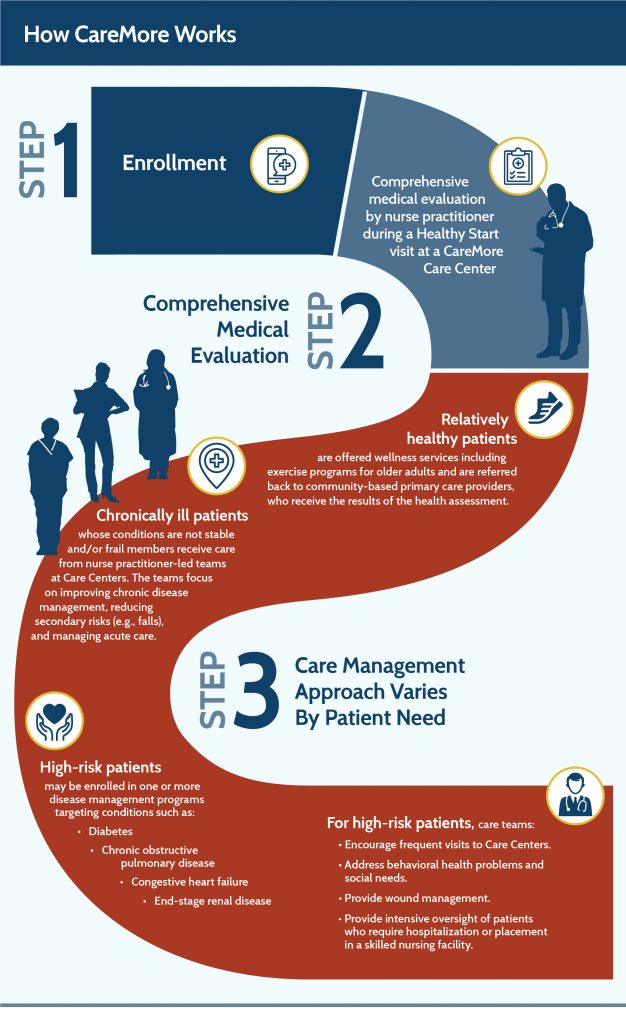 By focusing on high-needs patients such as those with end-stage renal disease, CareMore has reduced patients’ hospitalizations as well as better managing other risk factors common with kidney disease like diabetes and high blood pressure.
By focusing on high-needs patients such as those with end-stage renal disease, CareMore has reduced patients’ hospitalizations as well as better managing other risk factors common with kidney disease like diabetes and high blood pressure.
CareMore has accomplished this by attending to peoples’ needs beyond the medical, helping to identify gaps in those social determinants of health and close those gaps that bolster peoples’ overall health — physical, mental, social. “All healthcare is social,” Dr. Sachin Jain, CEO and President of CareMore Health, wrote about the latter in Forbes in April 2018 — and his essay is worth reading if you missed it the first time around.
And so the modern house call enables more social care, the CareMore model shows us. Home is indeed the hub of health, as I concluded in my book, HealthConsuming: From Health Consumer to Health Citizen: “Technology won’t be the barrier to bringing out health home. Public policy, lagging regulations, political will and personal commitment are the obstacles to people engaging in a new deal for self-care” at home.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.