“We knew millions of people weren’t getting the care they needed — they were either too embarrassed to seek help or felt stuck in a system that was confusing and intimidating. Digital health has the potential to radically change the way people approach their wellness and, since launching in 2017, we’ve outpaced even our own expectations, delivering more than 1 million Hims & Hers products to our customers. In collaboration with highly-qualified doctors and healthcare providers, we’ve built a digital health platform that is changing the way people talk about and receive the care they need.”

That’s a verbatim paragraph from a blog on the Hims & Hers’ Medium channel. published on 30 September 2019.
As we approach this coming weekend’s SelfCare Summit sponsored by GMDC, I continue to update my retail health ecosystem graphics and landscape. This post will be my latest read on the issue which I’ll discuss on Friday afternoon 5th October in a session titled, “The New Health/Care: Patient-Led, Retail-Enabled.”
Over the past sixty days, the business rationale for “getting people the care they need” could have been written into press releases from Sam’s Club and Walmart, Amazon, Best Buy and GoodRx, all of which announced plans in the past few weeks to extend health/care services in the U.S. beyond hospitals and bricks-and-mortar doctors’ offices.
Start with Hims and Hers, moving in the opposite direction from telehealth care focused on men’s and women’s health, morphing into a physical pharmacy distribution model. Hims and Hers will invest in a Columbus, Ohio-based mail order pharmacy to be operational in 2020, featuring customer support and fulfillment centers. Up to now, the companies have been working with third-party pharmacies to pick-and-pack medicines for consumers looking to support their gender-specific wellness needs.
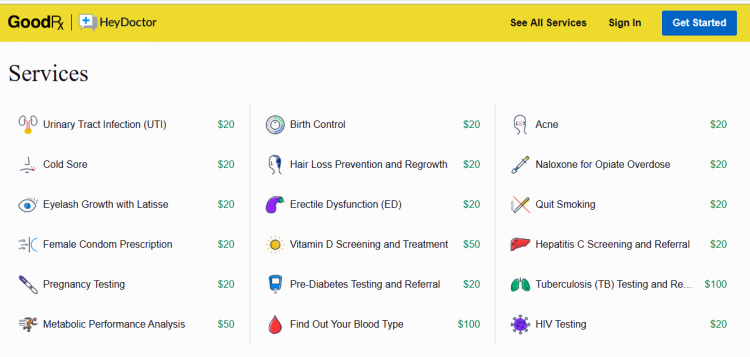
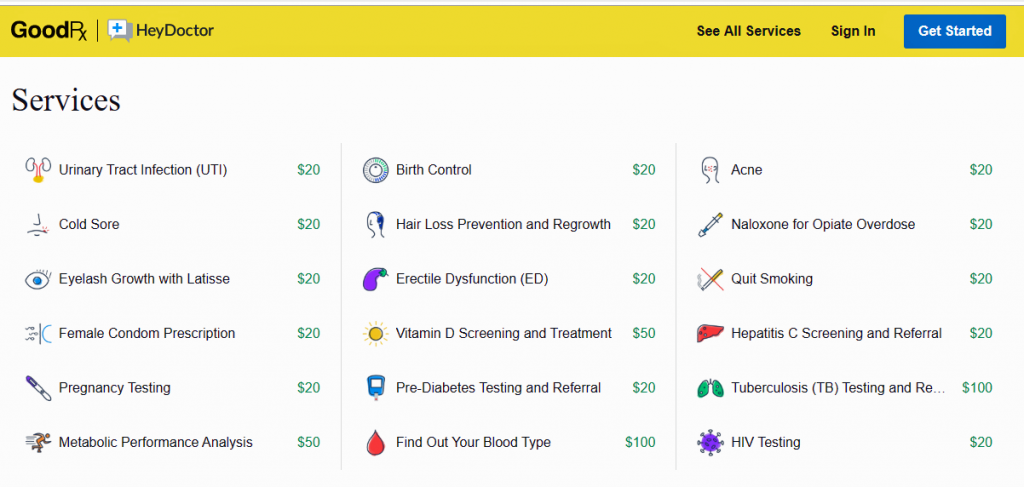 Now consider GoodRx, linking up with HeyDoctor to help the prescription drug discounting platform expand telehealth services. The organization will be known as GoodRx Care.
Now consider GoodRx, linking up with HeyDoctor to help the prescription drug discounting platform expand telehealth services. The organization will be known as GoodRx Care.
The press release announcing the acquisition of HeyDoctor on 26th September noted that, “This new service comes at a time when Americans find that getting access to primary care physicians to be increasingly difficult….As healthcare costs continue to rise and many insurance plans cover fewer services than they did a year ago, consumers need affordable options for their routine health needs. With the introduction of GoodRx Care, Americans now have easy access to a network of qualified medical professionals so they can get the treatment they need, when they need it….GoodRx Care aims to help fill in the gaps in care to improve access, adherence, and affordability of medical care for all Americans.”
HeyDoctor branded itself as an online urgent care provider with an app that’s generated good word-of-mouth among users. Among its most-used services are help for urinary tract infections, birth control, acne and cold sores, giving you an idea of the organization’s key (young) demographic.
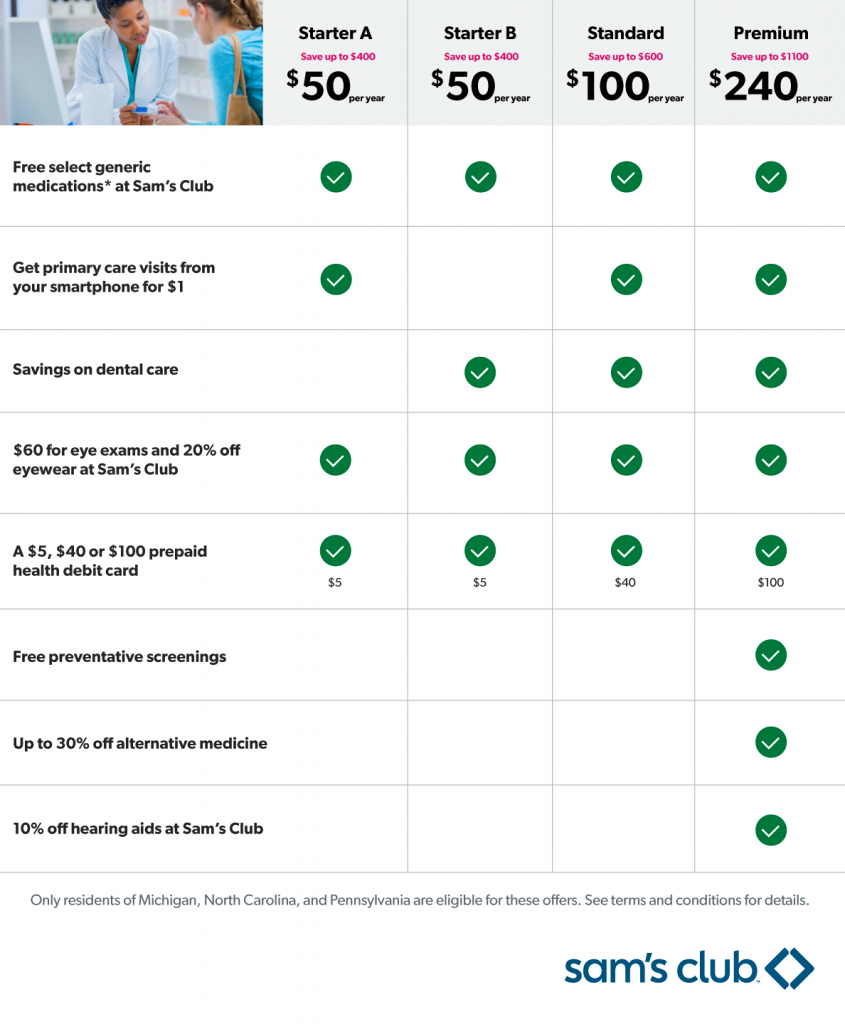 Addressing the access and affordability pillars, Sam’s Club launched a collaboration with Humana called Care Accelerator. As the third graphic illustrates, consumers can opt into one of four health care “bundles,” including components such as generic medications, primary care, vision and dental care, hearing and alternative medicine services. This isn’t meant to be a fully-loaded insurance plan, but a product that “curates” selected medical services consumers want to access at relatively low-cost to care for basic health care needs.
Addressing the access and affordability pillars, Sam’s Club launched a collaboration with Humana called Care Accelerator. As the third graphic illustrates, consumers can opt into one of four health care “bundles,” including components such as generic medications, primary care, vision and dental care, hearing and alternative medicine services. This isn’t meant to be a fully-loaded insurance plan, but a product that “curates” selected medical services consumers want to access at relatively low-cost to care for basic health care needs.
As I often say, “collaboration is the new black” in health care, and the Care Accelerator program brings together different partners to deliver components of care to the packages: in addition to Humana, Sam’s Club is working with Quest Diagnosis for lab testing and 98point6, an on-demand text-based app for primary care consultations. The 98pointsix primary care virtual visits cost $1 per visit and are included in the lowest-priced program at $50 per year, which also includes free select generic drugs sourced at Sam’s Club pharmacies, and discounted eye exams and eyewear.
The program is being piloted in Michigan, Pennsylvania and North Carolina and if it’s found viable and consumer-loved, Sam’s Club will expand it to club members across the U.S.
Programs range from $50 to $240 a year for the most complete plan. That $240 plan covers up to six family members and includes a preventive health screening looking at diabetes and heart disease.
Note that Sam’s Club is part of the Walmart business family, which has been fast-expanding its footprint in health care and wellness in the past several months. I’ve addressed the company’s growing health/care ethos here in Health Populi in these posts written this year —
Walmart’s Growing Footprint in Health/Care, from Guns to Mental Health and Gardens
FANGs & MAGA – Meet WaWa for Health, Walgreens and Walmart
How Walmart Could Bolster Healthcare in the Community
And for historical perspective, this post published over a decade ago in 2008!
.
 Finally, Amazon announced Amazon Care, its first clinic for employees in the headquarters Seattle area. This is not so much Amazon hanging up a brick-and-mortal medical center-shingle (like Walmart’s recent launch of a freestanding clinic model) but a hybrid of virtual care and in-person services.
Finally, Amazon announced Amazon Care, its first clinic for employees in the headquarters Seattle area. This is not so much Amazon hanging up a brick-and-mortal medical center-shingle (like Walmart’s recent launch of a freestanding clinic model) but a hybrid of virtual care and in-person services.
The Los Angeles Times analogized Amazon Care‘s disruptive to health care providers to Amazon Prime up-ending the retail shopping landscape.
It’s important to call out the technology media’s interest in this development: here’s Computerworld‘s take on the project, titled Why Amazon Care May be the New Model for Corporate Healthcare. Beyond the obvious link between Amazon as a tech company and the Haven alliance between AMZ, Berkshire-Hathaway and JPMorganChase, Computerworld mentions Apple’s AC Wellness concept for employee health clinics and smart businesses’ tighter focus on healthcare spending as, “a wake-up call for providers, payers and employers…(ushering in) a new operating system for health, and big technology companies are not going to wait for everyone else to figure it out.”
 Health Populi’s Hot Points: Stay tuned to my tweets @HealthyThinker and posts here on Health Populi between Thursday 3rd through Saturday 5th October as I listen to and learn from fellow speakers at the GMDC SelfCare Summit. We’ll cover a wide range of topics, from the future of retail health channels and trends, health plans’ approaches to inspiring members in self-care, new pharmacy formats, food-as-medicine, and consumer self-care forecasts.
Health Populi’s Hot Points: Stay tuned to my tweets @HealthyThinker and posts here on Health Populi between Thursday 3rd through Saturday 5th October as I listen to and learn from fellow speakers at the GMDC SelfCare Summit. We’ll cover a wide range of topics, from the future of retail health channels and trends, health plans’ approaches to inspiring members in self-care, new pharmacy formats, food-as-medicine, and consumer self-care forecasts.
I’ll be focusing on the patient-as-payor with high expectations for service and support for self-care health care for ourselves, our families, and in our communities.
Immediately following the SelfCare Summit, I’ll fly from Indianapolis to Kansas City where I’m delighted to meet with the Cerner user conference to brainstorm health consumers and healthcare costs in the context of health IT, revenue cycle management, and the patient-as-payor. Stay tuned to my tweets and posts there on Monday and Tuesday, 7th and 8th October.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.