One universal experience health systems around the globe have witnessed in the first months of the coronavirus pandemic has been the dramatic pivot to telehealth and virtual care platforms. The latest report from Philips Future Health Index series attests to that, and to clinicians’ general recognition that telehealth has been crucial in the early phase of the crisis.
However, younger doctors’ experience with telehealth has led to them being more bullish on the value of the modality than older physicians, Philips learned.
 Philips conducted 500 interviews with doctors in China, France, Germany, Singapore, and the United States to assess their views on technology and health care in the pandemic.
Philips conducted 500 interviews with doctors in China, France, Germany, Singapore, and the United States to assess their views on technology and health care in the pandemic.
The top-line findings across the five countries were that,
- Younger physicians remain, mostly, committed to the profession in the crisis
- Collaboration is a top priority for doctors
- Telehealth in the pandemic was, in Philips’ words, “crucial but underused”
- Interoperability is still an obstacle, and,
- Digital technology will be pivotal in the next few years.
In the first six months of the pandemic, the tale of telehealth as told via media coverage and virtual conference content has been quite bullish.
 From physicians’ point-of-view, telehealth has emerged crucial for delivering patient care and enabling a collaborative culture among doctors, but there remain concerns about the experience of using virtual care platforms for both clinician-to-clinician care as well as clinician-to-patient care.
From physicians’ point-of-view, telehealth has emerged crucial for delivering patient care and enabling a collaborative culture among doctors, but there remain concerns about the experience of using virtual care platforms for both clinician-to-clinician care as well as clinician-to-patient care.
More younger doctors recognize the “immediate value” of telehealth, Philips found:
- 61% of younger doctors said telehealth was among the top digital health technologies that would have most improved their experience during the pandemic.
- 53% of younger doctors said AI would have improved their pandemic experience.
Philips presented more granular data for each of the five countries studied. I show the findings for the U.S. here in two slides from the report.
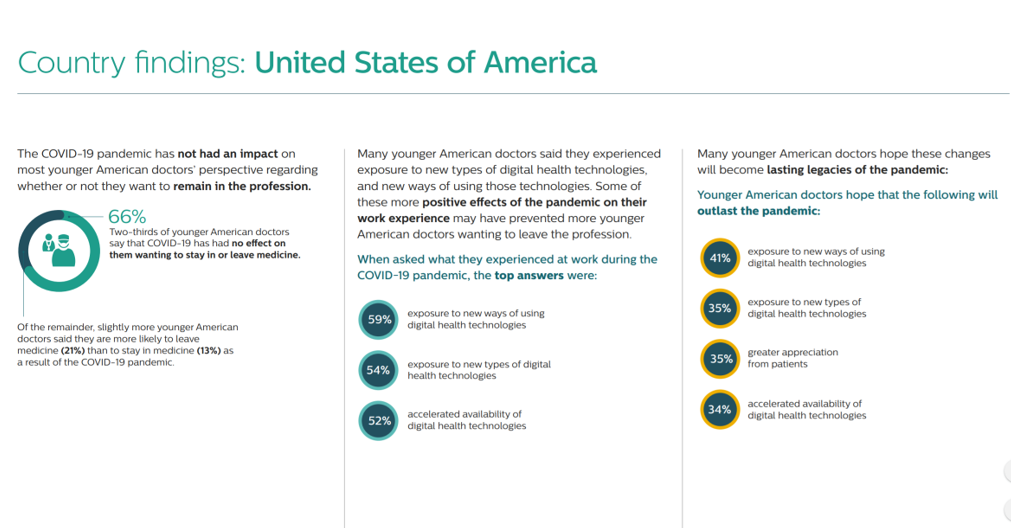
The first chart of U.S. findings covers young doctors’ views on the profession and work experience during the pandemic. Two-thirds of younger physicians said that their work during the COVID-19 crisis did not impact them wanting to remain in the medical profession. Of the remaining one-third, 2 in 3 told Philips they would be more likely to leave medicine, with 1 in 3 saying they would stay in practice.
Most younger physicians saw positive effects of using technology during the pandemic, bolstering their interest in remaining in medicine.
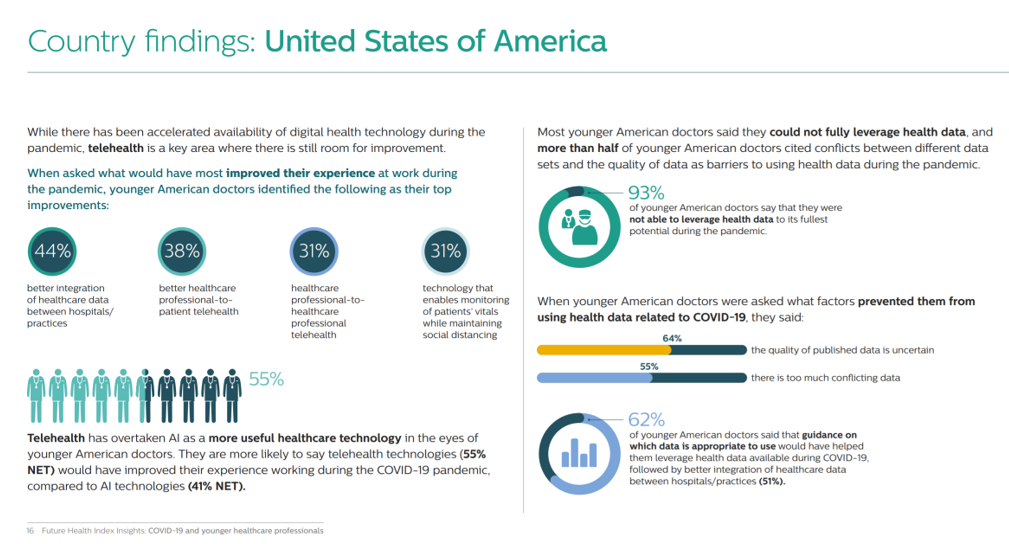
In the second chart on U.S. country findings, note that 93% of younger doctors were unable to fully leverage health data to its full potential in their workflow during the pandemic. Over one-half of doctors said there were conflicts between different data sets and quality of data, presenting barriers to the most effective use of data in the crisis.
 Health Populi’s Hot Points: Interoperability of data and systems were an obstacle in the first six months of the pandemic and remain an obstacle, most younger doctors observed. Philips discovered this in a previous Future Health Index study, which revealed that the portability of healthcare data between providers in hospitals and practices was a factor that would improve doctors’ work satisfaction.
Health Populi’s Hot Points: Interoperability of data and systems were an obstacle in the first six months of the pandemic and remain an obstacle, most younger doctors observed. Philips discovered this in a previous Future Health Index study, which revealed that the portability of healthcare data between providers in hospitals and practices was a factor that would improve doctors’ work satisfaction.
Philips Chief Medical Officer Jan Kimpen observed, “Healthcare professionals…have experienced unprecedented level of stress and were often faced with limited resources in recent months. We must acknowledge the heroic sacrifices that front-line healthcare professionals have endured in the fight against COVID-19. We owe it to them; to listen to their voices as we consider the future of the healthcare industry.”
Physicians and nurses began the calendar year 2020 with a great degree of emotional burnout, anxiety and depression, the 2020 Medscape National Physician Burnout and Suicide Report warned. The COVID-19 pandemic has not only been a crisis in terms of the virus itself, but a chronic burden of physical and mental health onus on clinicians on the front-line of care, and their families.
As Jan Kimpen recommended in the quote here, we owe it to clinicians to listen to their voices when re-imagining how to better rebuild the healthcare industry. The future of the hospital is at-risk in terms of fiscal viability, the American Hospital Association has warned in its revenue forecast for the remainder of 2020. For physicians, the hit is and will continue to be more than financial: it will be physically exhausting and emotionally taxing.
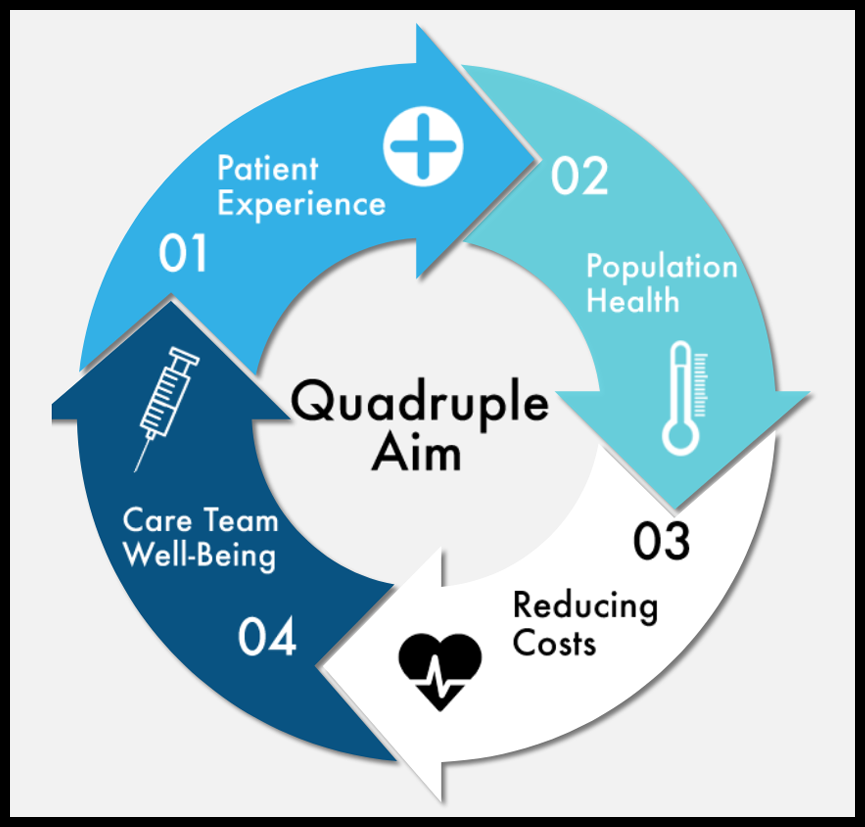
Technology solutions meant for clinicians to use must be designed to be productive, efficient, and even enchanting. The Philips Future Health Index names AI and telehealth as two main tech’s in physicians’ hands during the pandemic. But this report paints for us a cautionary tale and message beyond AI and telehealth — for all applications focused on clinical care used by our front-line professionals. Our health care system is only as strong as the clinicians who have been trained and committed themselves to serve it. That fourth leg of the Quadruple Aim stool must be strong, resilient, and supported to ensure a sustainable, effective health care system.
Today, 9/11. our empathy, love and appreciation go out to the heroic front-line health care workers in all generations, from 9/11 to COVID-19. Many of those who rushed to help on September 11, 2001, are, today, supporting COVID-19 efforts as highlighted in this Wall Street Journal story.





 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.