Health and our health information are deeply personal. Changing health care and inspiring positive health behaviors is hard to do.

But we must and we will, a group of inspiring and inspired people who work across the health/care ecosystem affirmed this week in Dallas at the conference of Medecision Liberation 2019.
I was engaged at this conference to wear several hats — as a keynote speaker, a sort of “emcee,” and, finally, to trend-weave the many talks and discussions happening throughout the meeting. This post is my synthesis of the summary I delivered live at the end of the conference, which one of the attendees described as “poetry slam-meets-healthcare.”
I quite like that new-and-improved Cliff’s Notes metaphor.
Deb Gage, Medecision CEO, kicked off the meeting. The inspiration started within minutes as Deb shared several personal stories involving the health care system and its flaws. Think of Deb as the proverbial shoe-maker’s child with no shoes: she leads a company helping drive digital transformation in health care, but two people she loved, and she herself, had all been failed by some aspect of fragmented health care delivery in America.
 Deb shared the experiences of Sam, her friend of 25 years, who had the quite-typical co-morbidity of multiple chronic physical conditions baked with mental health issues. Deb’s Dad, Ray, having lost his wife (Deb’s mom), was living alone, aging with some common conditions that come with living long and well, and wanting to stay independent in a health-and-social environment that doesn’t make this so easy to do. And Deb herself, surviving a tough condition, found that her own medical records were located in four disparate health systems based on the fragmented nature of her care delivered through different provider organizations.
Deb shared the experiences of Sam, her friend of 25 years, who had the quite-typical co-morbidity of multiple chronic physical conditions baked with mental health issues. Deb’s Dad, Ray, having lost his wife (Deb’s mom), was living alone, aging with some common conditions that come with living long and well, and wanting to stay independent in a health-and-social environment that doesn’t make this so easy to do. And Deb herself, surviving a tough condition, found that her own medical records were located in four disparate health systems based on the fragmented nature of her care delivered through different provider organizations.
Her learning, and ours: “We don’t need new tech….we need a single person view.”
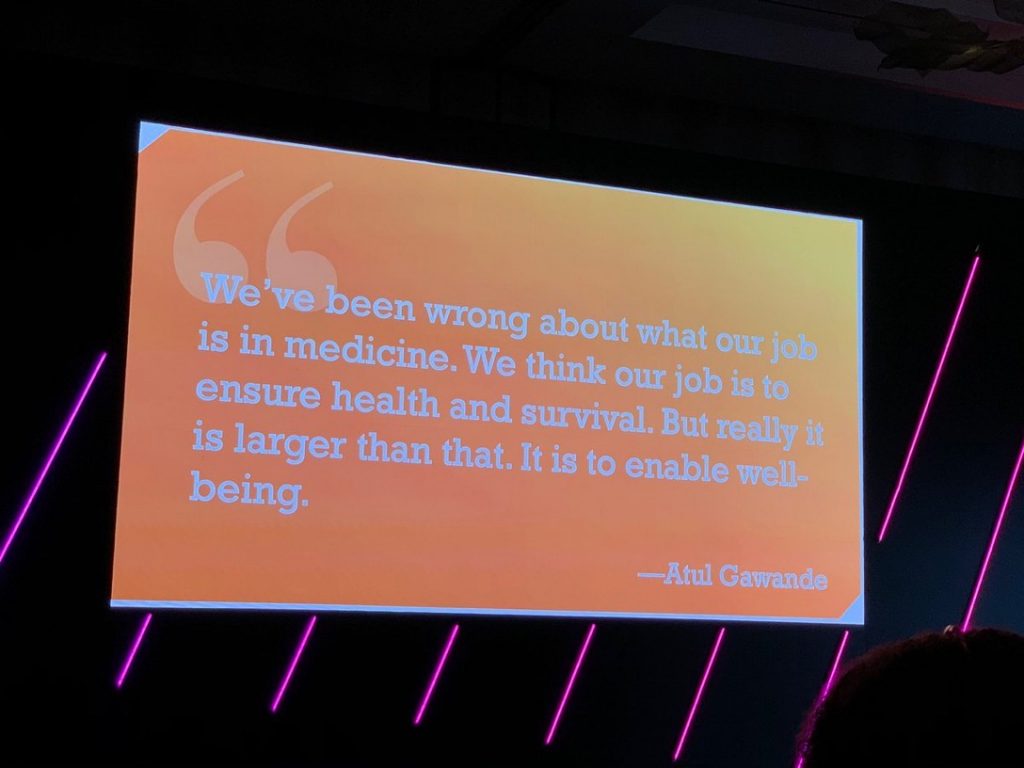
Furthermore, Deb pointed to this quote from Dr. Atul Gawande — that our job is not to ensure health and survival…it’s to enable well-being.
This ethos echoed throughout the 36 hours of Liberation 2019, culminating with the mantra of Nick Adkins, Co-Founder of the #PinkSocks Life community, who challenged us to look each other in the eye in close personal space to a new acquaintance and say (and mean), “I see you.”
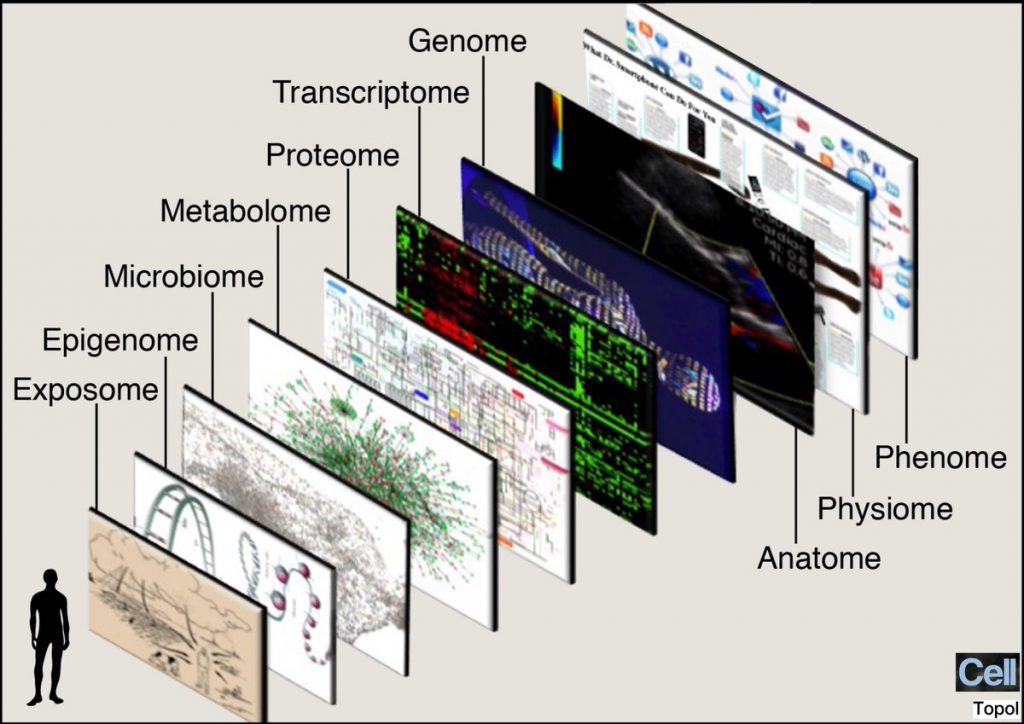 Another riff on “I see you,” that N of 1 person-patient-consumer, was Dr. Eric Topol’s explicit mission for Deep Medicine: that is, to personalize treatment based on evidence, not on the long-accepted
Another riff on “I see you,” that N of 1 person-patient-consumer, was Dr. Eric Topol’s explicit mission for Deep Medicine: that is, to personalize treatment based on evidence, not on the long-accepted
“sclerotic” medical thinking and prescriptions (as in “athero-sclerosis” blocked arteries) that aren’t based on the latest sound science. Dr. T’s “omes” slide, included in his book Deep Medicine, illustrates the many layers of a human being on multiple levels. I found this to be an apt metaphor once again for thinking about the individual human with many layers and lenses…the complexity of the individual with whom we must “go deep”
My own talk on the acronym I coined for this event, “TiSH,” spoke to each of our challenges with Trust, Stress, and Health Literacy. Taken together, these can be a toxic cocktail when not aligned for positive health behavior. Stress in America today crosses socioeconomic strata when it comes to health care costs several research studies have found that I cited, including surveys from the American Psychological Association and the Kaiser Family Foundation.
The call-to-action Rx for this is to get to know a patient’s values in terms of the life-flows and personal goals, as well as their “value” for health care — the ability and willingness to pay, their personal definition of affordability, and how that plays into their potential or actual self-rationing behavior due to cost. As many as 1 in 2 Americans has avoided some aspect of health care due to cost in the past year, such as postponing a needed visit to a doctor or not filling a prescription drug.
 So we’ve spoken to the N of 1 patient-person and the N of 1 physician-clinician. But if we want to change health care for the better, we must look into the eyes, Nick Adkins-style, of workers in health care. Chris Mahai, who runs Aveus, Medecision’s consulting division, wrote the book BOLD on leadership. The acronym stands for, “Believe, be Open, Learn, and Do.” Bold leadership, Chris and her panel who represented three different roles and health industry segments all believe that leadership can and should be fostered, embraced and rewarded at all levels of an organization. I was particularly struck and resonant with one of the panelists’ personal approach to change-agency at work: she said she tries to disrupt her work and workflows every day. That takes bravery, risk-management, and vision. And her organization’s top leadership supports her bold approach.
So we’ve spoken to the N of 1 patient-person and the N of 1 physician-clinician. But if we want to change health care for the better, we must look into the eyes, Nick Adkins-style, of workers in health care. Chris Mahai, who runs Aveus, Medecision’s consulting division, wrote the book BOLD on leadership. The acronym stands for, “Believe, be Open, Learn, and Do.” Bold leadership, Chris and her panel who represented three different roles and health industry segments all believe that leadership can and should be fostered, embraced and rewarded at all levels of an organization. I was particularly struck and resonant with one of the panelists’ personal approach to change-agency at work: she said she tries to disrupt her work and workflows every day. That takes bravery, risk-management, and vision. And her organization’s top leadership supports her bold approach.
During Liberation 2019, there were many moments of inspiration, but none more visceral or personal than the family history shared by Gary Mendell, founder of Shatterproof. Gary’s son was addicted to opioids and ultimately, after many months of being clean, took his own life. Gary’s mission with Shatterproof has four pillars, none more important than de-stigmatizing mental health and especially addiction by recognizing that it’s a legitimate healthcare condition worthy of parity of treatment priority and payment just like physical conditions such as cancer or heart disease.
 Gary talked of a vision, “that our society would look this straight in the eye, prevent, treat with love and empathy and with programs based on science.” This vision weaves together elements shared in the conference by all of the speakers, with Gary’s family’s learning this in the most personal, devastating way.
Gary talked of a vision, “that our society would look this straight in the eye, prevent, treat with love and empathy and with programs based on science.” This vision weaves together elements shared in the conference by all of the speakers, with Gary’s family’s learning this in the most personal, devastating way.
From Gary and the challenge of addiction, we moved and were moved by Dr. Shoshana Ungerleider’s leadership of Endwell, an organization devoted to expanding the concept of a good death. The U.S. fails in this end-of-life patient and family experience, and so many of us in the room where Shoshana shared her mission-driven message nodded, teased up, shook our heads, and stared this truth in its face. In Shoshana’s introductory video, a doctor from Stanford said, “Coming here (to the Endwell meet-up) and dealing with end of life makes me proud to be part of health care.”
There’s nothing more personal than one’s own death, and Shoshana challenges the siloed health care system to break down the siloed of home care, hospice, inpatient care, physician care, faith-based organizations, and disease advocacy groups to come together for the benefit of streamlining and humanizing death to make it just as enlightened a patient experience as other aspects of health care on life’s continuum.
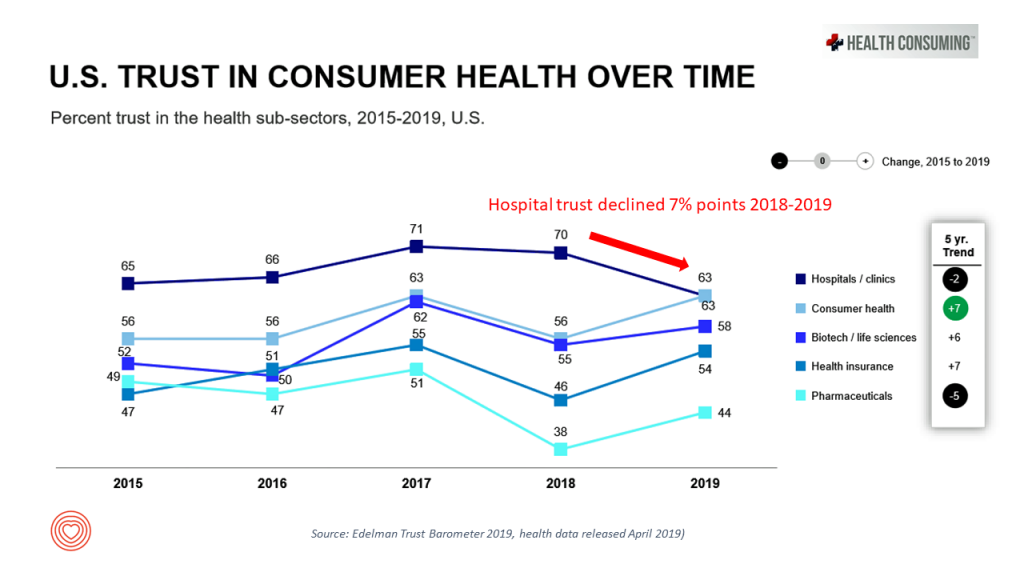 Patients and families who have felt betrayed by the health care system, as Gary and many of Shoshana’s communities, may have reacted, must feel trust again with those segments of the health/care ecosystem from whom they are alienated. Trust is a precursor for health engagement, and Lynn Hanessian and Cydney Roach of Edelman did a deep dive into the 2019 Edelman Trust Barometer. This year’s study, released as usual at the World Economic Forum in January, found that while overall trust in health care grew over the past year, there was a significant decline in trust in the hospital sector. Hospitals have traditionally been valued members in patients’ communities, with hospital beds notoriously difficult to close due to these institutions being so prominent in their towns and among the largest employers — economic engines — in their local geographies. But how the mighty have fallen in trust — even these pillars of local Chambers of Commerce and economies.
Patients and families who have felt betrayed by the health care system, as Gary and many of Shoshana’s communities, may have reacted, must feel trust again with those segments of the health/care ecosystem from whom they are alienated. Trust is a precursor for health engagement, and Lynn Hanessian and Cydney Roach of Edelman did a deep dive into the 2019 Edelman Trust Barometer. This year’s study, released as usual at the World Economic Forum in January, found that while overall trust in health care grew over the past year, there was a significant decline in trust in the hospital sector. Hospitals have traditionally been valued members in patients’ communities, with hospital beds notoriously difficult to close due to these institutions being so prominent in their towns and among the largest employers — economic engines — in their local geographies. But how the mighty have fallen in trust — even these pillars of local Chambers of Commerce and economies.
Julie Murchinson, CEO of Health Evolution, concluded the meeting with her insights into “tribes.” She noted that each of us, within and outside of health care, but each of us people is a member of a tribe that’s unique to us, riffing on the work of Dave Logan. Some of us are in tribes where we feel we’re great (and “you’re not”). Some of us are in tribes where we feel marginalized by society and hang with other people in our tribes who feel the same way. Some of us feel communal in our tribe in that our operating system is inclusive for the whole versus the individual in and of ourselves. Recognizing that we are all in tribes, sometimes quite different than the ones with which we identify.
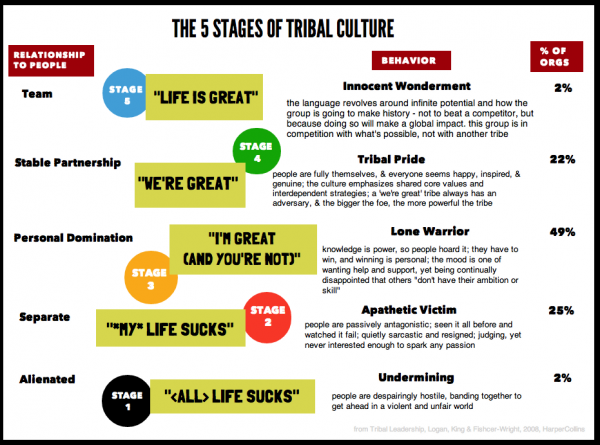 Julie’s call-to-action asked each and all of us: “How do we drive change in health care as a tribe to make a movement?”
Julie’s call-to-action asked each and all of us: “How do we drive change in health care as a tribe to make a movement?”
She pointed to Greta Thunberg, who at 16 has indeed inspired a movement to popularize climate change across borders, age groups, social strata, and political persuasions.
Greta is as good an inspirational role model as any we can channel in these cynical days.
That’s liberating. That’s Liberation 2019.
Thank you, Medecision team, for convening this exciting, inspiring, informative meeting. This isn’t my job at moments like this; it’s a mission.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.