Automated Insulin Dosing — Past, Present and Future
The artificial pancreas is a dream that is slowly coming true. We thought it would be useful to review where we are and where we might be going.
The ultimate goal of Automated Insulin Dosing (aka artificial pancreas) requires sensing BG levels, then calculating and delivering insulin in an ongoing feedback loop. There is a wide range of approaches to achieving this, and one would think that it’s a relatively new innovation in recent devices, but that is not the case.
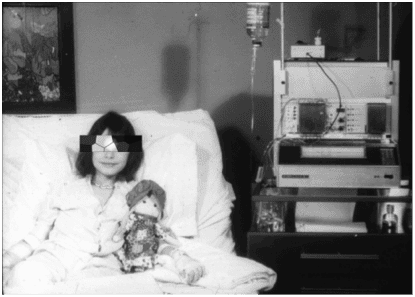
The idea for such a system was pioneered in 1964, and the first commercial device, the Biostator, was introduced in 1977.
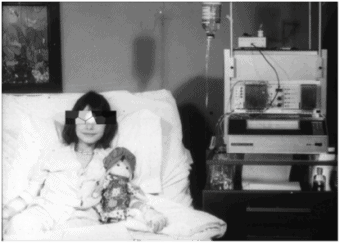
The system was a large device that sat at a patient’s bedside in the hospital. While the device broke the mold, it had serious limitations with the amount of oversight required and oversimplified glucose management algorithm, or calculation.
As we look at the future of automated insulin dosing, what will set devices apart and make the artificial pancreas more successful are the algorithms in devices that recommend an appropriate insulin dose based on each patient’s unique factors. Like the Biostator, we can again look to insulin dosing tools and the algorithms used within the hospital setting for what future devices may hold.
Inpatient insulin dosing systems, or eGlycemic management systems, have replaced paper protocols and have become best practice in top hospitals. Some hospitals have just computerized the paper protocols, but others have incorporated more complex algorithms for precise insulin dosing. For example, EndoTool from Monarch Medical Technologies (website) has helped hospitals and their patients rapidly achieve BG targets while virtually eliminating hypoglycemia. It gathers inputs from the electronic medical record and from clinical professionals to provide a recommended dose to the clinical professional to administer. In addition to BG levels and carbohydrates, these extra inputs include steroid levels and kidney function.
We interviewed Monarch EVP and Chief Clinical Officer Laurel Fuqua, RN, MSN, who did early work with the Biostator, to gain insight into the future of automated insulin dosing.
“Our inpatient dosing algorithms are finely tuned to the individual patient, and thus, are more precise in maintaining in-range BG levels. One indicator of this tuning capability is that Monarch uses more than 70 algorithm decision points in its insulin dosing system.”
Precise insulin dosing is important, and damage accumulates when it’s not done well. A recent Swedish T1D mortality study found that living with T1D often results in 10-15 years less total lifetime compared to non-T1D people because of all the complications due to out-of-range BG control.
While the insulin dosing support in the outpatient setting has typically been comprised of simple insulin dosing calculators, this is rapidly changing. In addition to devices that can recommend basal or bolus insulin doses, there has been tremendous progress in the mechanics of BG sensing and insulin delivery. CGMs and pumps are smaller and are now integrated with mobile devices. BG sensors are smaller and are effective for longer periods. Insulin delivery methods are more refined and trouble-free.
Additionally, the utilization of more sophisticated algorithms within devices has already begun. Medtronic led the way in 2016 with its MiniMed 670G Insulin Pump System. Dexcom just acquired TypeZero, the algorithm supplier to Tandem’s recently introduced t:slim X2 Insulin Pump with Basal-IQ Technology, and promises a smarter CGM using TypeZero algorithms in 2019. Insulet also seems on its way to a 2019 pump with a smart insulin dosing algorithm.
In the T2D space, Monarch has partnered with Voluntis (release) to improve outpatient T2D basal insulin dosing. Basal insulin therapy is often used in combination with other diabetes medications in T2D and self-adjustment of basal insulin has been shown to be effective. Digital tools, like Insulia, have algorithms that provide patients with daily recommendations for how much insulin to take based on their BG and insulin prescription.
Ellie Strock, Vice President of US Medical Affairs at Voluntis said “The most recent standards of medical care in diabetes indicate the need to equip people with diabetes with an algorithm for self-titration of insulin. Insulia incorporates these algorithms to titrate basal insulin and allows people with type 2 diabetes to take a correct dose of insulin every day.”
As with all new innovation and technologies, however, adoption can be slow. For example, adoption of CGMs and pumps has been more modest than we would have expected with only about 10% of potential users having one or more of the devices. Many PWD people still feel they can manage their BG with just meters and injections.
Smart algorithms built into more consumer-friendly devices may change this equation. With more precise dosing, less maintenance, and ease of mind in managing BG, patients may finally get their dream of a successful artificial pancreas.