New Study Reveals Importance of CGMs in Diabetes Management
New technology helps millions avoid dangerous complications of diabetes but CGMs are most important in achieving optimal blood sugar control
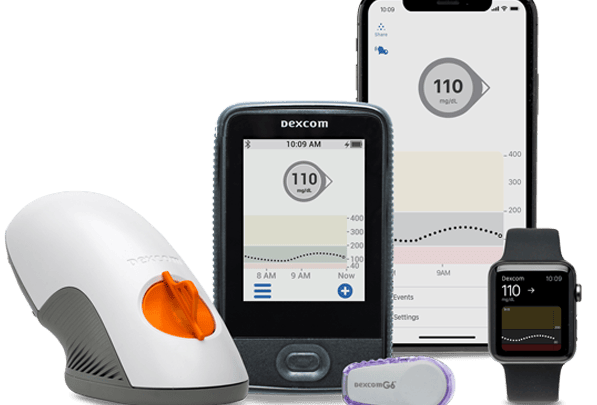
A recent study published in Diabetes Care compared the A1Cs and time-in-range of people who used finger pricks to test their blood sugar against those using a continuous glucose monitor (CGM). Each group was followed for three years, with statistics gathered throughout.
Researchers found that regardless of the method used for insulin injection, MDIs or insulin pumps, patients who used a CGM had an average decrease of 1.3 in their A1C, an average increase of five hours a day for time-in-range, and a decrease of one hour per day spent below range.
If you have experience with a CGM, it probably isn’t surprising to find out that using one results in tighter blood sugar control. But what is surprising about this study is how much more powerful the effect of the CGM was over the method of insulin injection.
A Real-to-Life Set-Up
In the COMISAIR follow up study, 94 adults, all with baseline A1Cs between 7 and 10 who did not have recent experience with using a CGM were chosen for this real-life, nonrandomized study. Each individual was given the choice of using a CGM or standard finger-prick glucose testing and the choice to use a pump or MDIs for insulin injection. Each participant picked the combination of management options that best suited their lifestyle.
One obvious concern about this non-random, participant-driven format is that those individuals who are more likely to put extra energy into their diabetes care might gravitate toward using a CGM. If this was the case, the results could be easily skewed in favor of CGM use because those individuals would be more motivated and therefore more likely to show improved A1Cs anyway.
However, the study’s authors are quick to point out that all participants had to commit to an intensive four-day insulin dosing training that would seem to prove that all members were motivated to manage their diabetes better. Additionally, I would expect those most motivated to improve their numbers would opt for the CGM and pump combination as these have traditionally been seen as the most effective way to manage the condition long term. But the results do not show a significant difference in stats between those with CGMs and pumps and those using CGMs with MDIs.
All participants were required to complete frequent clinic visits early on, followed by visits every three months for the full three-year study. Data from CGMs and meters were downloaded and other data were collected from pumps or self-reported.
Surprising Results
All participants received training on insulin dosing amounts and timing, as well as encouragement to check blood sugars more frequently (if not on a CGM) and make adjustments in basal or long term insulin doses as needed.
Thus, it is no surprise that an immediate drop in A1Cs was noted across all groups.
At three months, the average A1C for the non-CGM group dropped from around 8.4 to about 8, while the CGM group dropped from 8.3 to 7.5. After that initial change, the non-CGM group leveled out with an average A1C around 7.85 while the CGM group continued to drop until around the 12-month mark and then leveled out around 7.
While this study clearly shows an advantage in managing diabetes with the help of a CGM, just as striking is the apparent unimportance of insulin pump use.
Within the group using CGMs, some chose to use MDIs while remaining members chose to use an insulin pump. Similarly, within the non-CGM group, some members chose to use a pump while the rest chose MDIs. The researchers found no statistical significance in the outcomes of each subgroup compared to their group as a whole. Meaning that using a pump in conjunction with a CGM did not result in more time spent in range or a lower A1C than MDIs paired with the use of a CGM. Likewise, using a pump without a CGM didn’t result in better glucose control than MDIs without a CGM.
Also worth noting, is that the members of the CGM group showed an increase in the average number of boluses given per day. This is likely a driving factor behind the improved A1Cs. But could also be evidence that participants wearing a CGM felt more comfortable eating more frequently, rather than waiting until after a post-meal blood sugar check. While both CGM subgroups showed a similar substantial increase in this stat, only the pump users in the non-CGM group showed a slight increase in the average number of boluses per day. Those on MDIs without a CGM showed no change at all.
So, while a pump may not be a vital tool for maintaining tighter blood sugars, there is some evidence that its ease of use allows for more frequent insulin injections and therefore acts as a tool to simplify diabetes management.
Takeaways From This Study
More type 1 diabetics should switch from finger-prick glucose monitoring to a CGM.
Having continuous information about blood sugar levels allows diabetics to make more informed choices around correction boluses, the timing of meals, and adjustments to basal levels. This not only reduces the frequencies of high blood sugars, which means fewer complications later in life but also reduces the risk of hypoglycemia-related emergencies.
But even more importantly, this study paints a clear picture of where resources and money should be pooled to increase positive outcomes for those with diabetes.
In a perfect world, all diabetics would have access to the life-changing technology that makes managing diabetes easier, more effective, or both. But, at least right now, while resources are limited for many who suffer from this condition, knowing what treatments offer the best chance at a positive outcome will help patients and prescribers make an informed decision based on their specific situation.