The Search for Value is the prevailing journey to a Holy Grail in healthcare these days. On that, most stakeholders working on the ground, globally. can agree. But whose value is it, anyway?
Three reports published in the past few weeks give us some useful perspective on that question, woven together in today’s Health Populi blog.
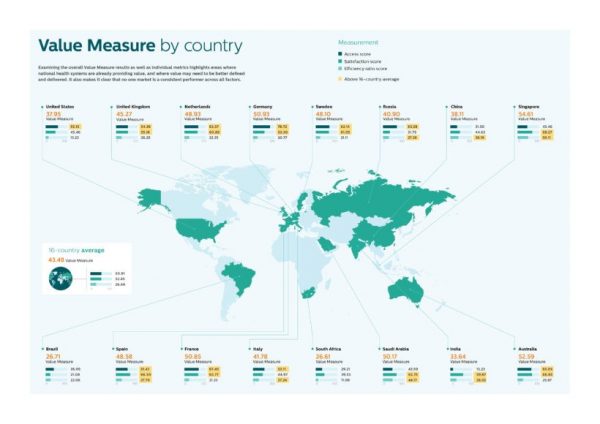
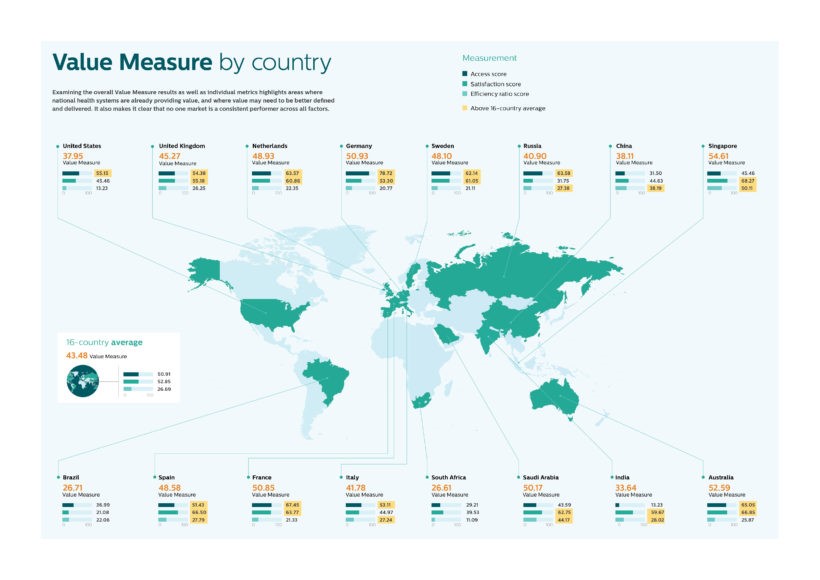 Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map.
Let’s start with the Philips Future Health Index, which assesses value to 16 national health systems through three lenses: access, satisfaction, and efficiency. The results are shown in the map.
“Value-based healthcare is contextual, geared towards providing the right care in the right place, at the right time and at the right level of cost,” the Index report defines. The U.S. overall scores below the 16 country average across the 3 measures, only above average for access.
“The US is a clear outlier,” the report explains. The key factors underneath the low Index score are low levels of satisfaction, where Philips found that only 40% of the U.S. population expressed trust in the healthcare system. In addition, efficiency, with the greatest spend of GDP on healthcare versus other nations, yield outcomes falling short of most of Europe, Australia, and Singapore.
The report quotes Nancy Brown, CEO of the American Heart Association: “Everyone [in the U.S.] knows the current system isn’t working. If you look at the places where the system is working, they’ve got it figured out, but that’s not the world the rest of healthcare and patients live in.”
The Index “winner” is Spain, which scores above-the-averages across all three metrics.
Interestingly, Russia scores overall better than the U.S. on value, where only satisfaction ranks below the U.S.
China’s Index of 38 is near-identical to America’s.
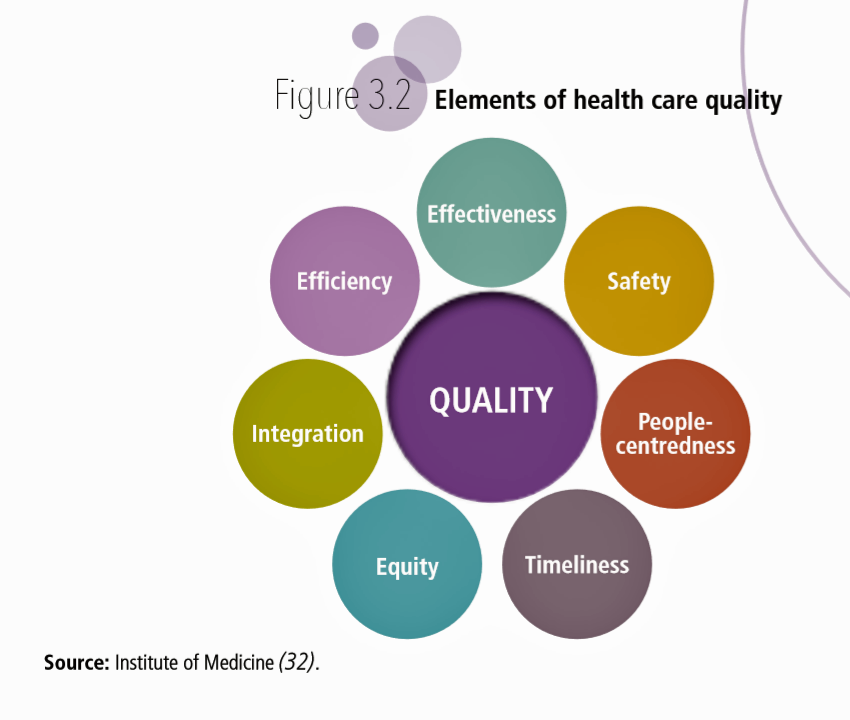 Another global view on value is offered in the report, Delivering quality health services: A global imperative for universal health coverage, from the World Health Organization, the World Bank Group, and the OECD. This report defines quality as, “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and consistent with current professional knowledge.” The way forward to bolstering outcomes rooted in the latest clinical learnings involves all healthcare stakeholders:
Another global view on value is offered in the report, Delivering quality health services: A global imperative for universal health coverage, from the World Health Organization, the World Bank Group, and the OECD. This report defines quality as, “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and consistent with current professional knowledge.” The way forward to bolstering outcomes rooted in the latest clinical learnings involves all healthcare stakeholders:
- Governments, who should have a national healthcare policy and strategy, a resilient information/technology infrastructure, partnerships between providers and patients/”users”, and value-based purchasing;
- Health systems, implementing evidence-based care, streamlined services to improve chronic care management, a do-no-harm culture, and learning infrastructures that facilitate information and knowledge-sharing;
- Health workers, sharing a practice philosophy of teamwork, embracing patients as partners in co-creating care, and using data to demonstrate effective and safe care; and,
- Citizens and patients, to be empowered to actively engage in care, to play a “leading role” in designing new models of care for their local communities, to receive support and skills to manage their own long-term conditions, and to be informed of their right to have access to care that meets modern standards of quality.
Teaming across and within these stakeholder groups — provider to provider to patient, government to health citizen, clinician to system to patient, and patients in peer-to-peer support — support what’s shown in the IOM circle drawing on quality elements: integration, equity, timeliness, safety, efficiency, effectiveness and ultimately people-centredness.
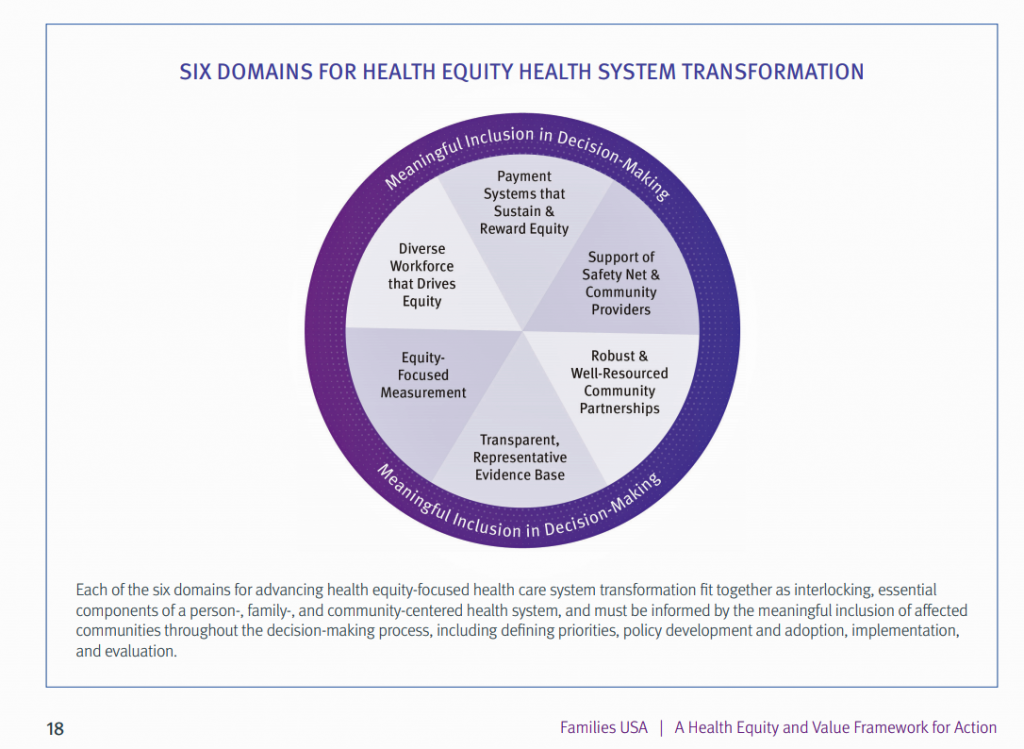 Families USA published A Framework for Advancing Health Equity and Value calling out health inequities in the U.S. health system that can result from value-based payment regimes. Families USA is “the voice for health care consumers,” so advocates on behalf of patients and caregivers.
Families USA published A Framework for Advancing Health Equity and Value calling out health inequities in the U.S. health system that can result from value-based payment regimes. Families USA is “the voice for health care consumers,” so advocates on behalf of patients and caregivers.
“Our health system is failing us,” the report’s summary asserts in its first sentence. The definition of opposite of value is in the second sentence: “As a nation, we spend too much and get too little in return.” A key aspect of that non-ROI is the extent and severity of health care disparities which are systemic and affect people of color, with lower-incomes, with disabilities, and living in distressed geographies.
As the U.S. evolves toward value-based payment, well-designed programs can address quality and access for people who have been left out of evidence-based, accessible healthcare. Key elements to consider here are examining how risk-adjustment accounts for clinical and social risk — or not; fair and efficient resource allocation to safety net, rural, and community hospitals; and, getting real about disparate impacts on particular communities. [This raises the issue of the U.S. Census and who will be counted in the macro numbers; that database is one of the major go-to’s for policy makers in making resource allocation decisions].
The solutions, Families USA recommends, are to design payment systems that sustain and reward quality, equitable health care; invest to support safety net and small community providers in health system reform; build robust community partnerships that are sufficiently resourced; ensure transparency and a representative evidence base; measure with equity focus in mind; grow a diverse health care workforce that drives equity and value at the same time.
Together, these three reports help us better understand the concept of value-based healthcare, from global to local communities where people can co-create health.
 Health Populi’s Hot Points: I’ll land on the side of the patient, consumer, health citizen weaving together the recommendations in these reports. There’s no reaching the elusive Quadruple Aim — driving health outcomes, enhancing the healthcare experience, supporting clinicians in their resiliency, and ultimately reducing per capita costs — without patients engaging in their own healthcare, self-care, and activation.
Health Populi’s Hot Points: I’ll land on the side of the patient, consumer, health citizen weaving together the recommendations in these reports. There’s no reaching the elusive Quadruple Aim — driving health outcomes, enhancing the healthcare experience, supporting clinicians in their resiliency, and ultimately reducing per capita costs — without patients engaging in their own healthcare, self-care, and activation.
This last graph comes out of the WHO/World Bank/OECD report: it illustrates consumers’ perceptions on whether their doctors provide easy-to-understand explanations. This is a proxy for positive patient experience at that “moment-of-truth,” in the space between doctor-and-patient where shared decision-making can happen….or not.
The U.S. result on this falls above the OECD average, but well below other nations whose populations enjoy far better health outcomes — and where far less money is spent, per capita on health care.
The sort of teamwork recommended in the report, across stakeholders, putting patients at the center of health system design, can help a statistic like this one move up the customer experience curve. Embedding systems that boost patient trust, satisfaction, and engagement have a hard ROI in moving outcomes and, thus, lowering healthcare costs.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.