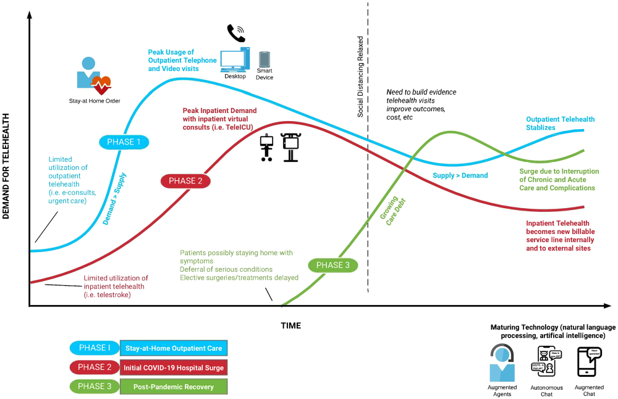
A recent study out of the Duke University Department of Medicine explored the role the COVID-19 pandemic has had on digital transformation in healthcare. The research discusses how COVID-19 has catalyzed telehealth and telemedicine adoption, forcing a digital transformation that is the new reality and here to stay. The researchers provide advantages and limitations of various telehealth modalities throughout the three phases (listed below) of the United States response to the pandemic, as seen at healthcare organizations across the US.
The researchers discuss telehealth’s role in three phases:
- Stay-at-Home Outpatient Care
- Initial COVID-19 Hospital Surge
- Post-Pandemic Recovery
Source: Duke University School of Medicine, 2020
Phase 1: Transition to Stay-at-Home Outpatient Care
Stay-at-home orders began in March 2020 in the United States. As of the date of this blog’s release, 18 states have on-going stay at home orders, and 30 have eased restrictions, allowing certain businesses to reopen. One hundred thirty million people across the United States are still under some form of lock-down. During this time, healthcare providers across the country have turned to telehealth to ensure that their patients can remain at home while still receiving the care they need. In addition, telehealth has helped keep both patients and providers safe during the pandemic by reducing the potential for community spread of the virus.
The Duke researchers discuss how US health systems had low rates of telehealth utilization for routine care prior to the pandemic, with those with ‘high’ telehealth adoption performing less than 100 video visits per day. Now, video and telephonic visits have replaced nearly all in-person visits. Forrester’s recent report found that, before January 2020, 24% of US healthcare organizations had a virtual care program. Now, their projection shows that by the end of 2020, virtual care visits will exceed 1 billion (900 million for COVID-19, 200 million for general care, and 80 million for mental health). Similar predictions have been made by other companies as well. For example, Frost & Sullivan predict a seven-fold growth in telehealth by 2025 - a five-year compound annual growth rate of 38.2%.
According to a recent study from NYU Langone, virtual urgent care visits grew by 683%, and non urgent virtual care visits grew by 4,345% between March 2 and April 14 within the health system. NYU Grossman School of Medicine researchers who led the study at NYU Langone found that over six weeks, 2,656 providers conducted 144,940 video visits with 115,789 unique patients.
At Duke specifically, telehealth visits increased over four weeks from <1% of total visits to 70% of total visits, with more than 1,000 video visits occurring each day. To manage the cumbersome shift, Duke created a centralized telehealth call center that is staffed by newly hired and repurposed staff, medical students, and “super users.” Duke embodied a “train the trainer model” which enables rapid staff development to onboard providers quickly.
Phase 2: Inpatient COVID-19 Surge & Tele-ICU
As demand for hospital-level care increases due to COVID-19, many healthcare organizations across the country are rapidly responding by deploying tele-ICUs. The tele-ICU approach allows staff (those in quarantine, those in high-risk groups, and those with childcare or caregiver responsibilities) to work remotely and supplement in-person clinical visits. For example, a pulmonologist can video into the patient’s room remotely and perform a video consultation.
Many health systems are deploying telehealth carts that have previously been used for telestroke. Others are clamping telehealth tablets on mobile structures and moving them around the hospital as needed, bringing the remote clinician to various settings.
For example, at Duke, a Tele ICU was established to allow specialists to manage intubated patients remotely. Physicians can view the ventilator settings, patients’ work of breathing, and remotely consult with the clinical team at the patient’s bedside. This modality decreases exposure to risk, preserves personal protective equipment (PPE), and facilitates easier access to more patients across multiple locations.
At Mount Sinai Health, clinicians watch streamed live footage of inpatient units and communicate with patients remotely, further reducing exposure to the virus. Similar to Duke’s experience, this has allowed Mount Sinai to preserve PPE, keep staff safe, and ensure every ICU patient is actively monitored at all times.
Phase 3: Post-Pandemic & The Future of Telehealth
This phase is the most uncertain, as it has not yet happened. Experts across the industry have predicted that telehealth is here to stay as a new standard of care delivery. Due to the pandemic, healthcare organizations across the country had to embody a digital health strategy in weeks and even days in some cases, a process that typically takes months or years.
The Duke authors explain that “health systems should work to create a strong, sustainable telehealth infrastructure now that will allow for more efficient use of hospital space and staff.” It’s essential that telehealth service lines are strengthened and grown between affiliate hospitals and providers. This is especially vital with rural and critical access hospitals to ensure that all patients have access to specialty care should they need it.The shift from crisis response to sustainable telehealth programs that abide by patient privacy standards and data security will be most reflective of the post-pandemic phase. The federal government has lifted many restrictions on telehealth delivery (for example, HIPAA and location regulations) that were previously barriers to telehealth and reimbursement has been expanded by Medicare. Most notably, the CARES Act (signed on March 27, 2020) eased telehealth regulations, allowing for increased flexibility in telehealth care delivery. Providers and patients are encouraged to opt for telehealth and the regulations, now more than ever before, support them in doing so.
What the Future Holds for Telehealth
Telehealth has emerged as a public health necessity, becoming a must-have across the care continuum. Due to social distancing rules, vulnerability, and the uncertainties of the virus, patients across the country prefer to stay at home and receive their healthcare remotely - in many cases, in-person care is not even an option. Providers have responded to the demand and have implemented telehealth and telemedicine modalities across their organizations.
Undoubtedly, we have entered the age of telehealth. The rapid digital transformation occurring now will lay the groundwork for telehealth in the future. We can assume that patients will continue to opt for care that mitigates risk and reduces unnecessary interactions. Individuals and providers now believe in and have seen the many values of telehealth - convenience, quality, cost savings, patient satisfaction, to name a few - and will trust it into the future as an effective way to deliver care.
Read the full study from Duke, here.
Read the full study from NYU Langone, here.