1 in 12 people across the nation depend on Federally Qualified Health Centers (FQHC) for care. FQHCs play a critical role in providing accessible, low cost care to patients, regardless of ability to pay. Traditionally, FQHCs have faced several hurdles in adopting telehealth including regulatory barriers such as lack of Medicare coverage. However, with FQHCs on the frontline of COVID-19, Congress and CMS have adjusted their policies to support FQHC expansion in telehealth. At HRS, we believe it is imperative to understand the importance of FQHC’s role in the care continuum, and we hope that policy changes continue to encourage telehealth adoption to further meet the needs of patients across the country.
What is a FQHC?
A Federally Qualified Health Center is a nonprofit, community-based, safety net provider that offers primary and preventive care. The goal of an FQHC is to provide care to underserved populations such as the uninsured, Medicaid, Medicare, SCHIP, migrant, homeless, other public health patients. FQHCs perform internal medicine, pediatric care, family practice, mental health care, and subspecialty care, similar to the services provided at a typical outpatient clinic.
To become an FQHC and receive funds from Health Resources and Services Association (HRSA), a patient care center can apply given it meets specific requirements. According to the Federal Health Center Program, a program can qualify as an FQHC if they meet the following specifications:
- Cannot deny any patient service, regardless of ability to pay
- Offer a sliding fee scale to accommodate different abilities to pay
- Qualify for enhanced reimbursement from Medicare and Medicaid
- Have a governing board of directors mostly composed of patients
- Serve a Medically Underserved Area or Population
- Provide comprehensive primary care services
- Have an ongoing quality assurance program
Importance of FQHCs in the Care Continuum
FQHCs play an essential role in a patient’s long-term care, especially in terms of access. Although FQHCs are commonly used interchangeably with RHCs, or rural health centers, the two differ in key ways. While both entities typically provide primary care services, RHCs are strictly located in rural areas. FQHCs are not defined by their location and can be found in either rural or urban areas. As a result, FQHCs can reach a broader range of patients, addressing the issue of access for many.
Furthermore, FQHCs typically provide more community and social services than RHCs. These services include case management, transportation, translation, nutrition and social worker services. According to a 2019 study from UnitedHealth Group, 2/3s of ER admissions amongst the privately insured are avoidable - this number is likely even higher when factoring in those publicly insured or uninsured patients, typically seen at an FQHC. Studies have shown that by providing access to primary care and case management, regardless of a patient’s insurance status and health condition, FQHCs defer patients from costly avenues of care such as the ER.
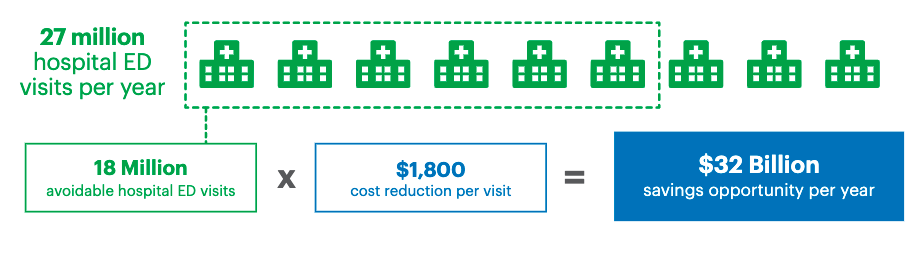
Source: The UnitedHealth Group, 2019
In addition to providing care to patients in all locations and reducing ER admissions, FQHCs play an important role in continuity of care. Regardless of medical, dental, or behavioral needs, the patient always has a medical home with an FQHC. This model encourages the development of ongoing relationships with clinical teams, resulting in continuous, integrated care. By serving patients of all ages, regardless of insurance or socioeconomic status, FQHCs target health disparities and work to empower underserved areas with low-cost, high-quality patient care.
COVID-19 Impact on Telehealth Services
Prior to COVID-19, there were several policies in place that prevented FQHCs from adopting telehealth services. With the onset of this public health emergency (PHE), CMS has temporarily added flexibility to policies for the duration of COVID-19 PHE to accommodate more patients during this time of need in these main areas:
1) Originating vs. Distant Site Designation
Before the pandemic hit, CMS allowed FQHCs to serve only as originating sites, or the location of the patient at the time the service is performed - typically a medical practice or facility. FQHCs were not allowed to be billed as a distant site, or the location of the practitioner at the time the service was performed. However, as of April 17th, 2020, under the Coronavirus Aid, Relief, and Economic Security Act (CARES Act), FQHCs can now act as a distant site to Medicare beneficiaries, thus allowing health center providers working from home to bill for those services as a “distant site” practitioner as opposed to receiving only the “originating site” facility fee. This change empowers providers by encouraging their safety in working from home.
2) Expansion of Virtual Communication Services for FQHC
Before the CARES act was enacted, CMS reimbursed solely for real-time synchronous audiovisual telehealth visits. The CARES act expanded the services reimbursed under virtual communication by introducing “e-Visits”. These online digital evaluation and management service codes reimburse for qualified non-face-to-face digital communications via secure patient portals that are initiated by patients and require a clinical decision. Currently, HRS partners with Zoom Health for seamless HIPAA-compliant multi-user audiovisual calls that would be qualified as a standard telehealth visit. However, HRS also has calling capabilities that allows the patient to speak to their clinical team without video, allowing for streamlined conversation. With this expansion, FQHCs can now be reimbursed for both types of communication.
3) Revision of Home Health Agency Shortage Area Requirement
Additionally, prior to COVID-19, CMS did not often reimburse telehealth services provided at the patient home unless the patient resided in a location with a shortage of home health agencies (HHAs). However, with the onset of the pandemic, CMS now considers all FQHCs as locations of HHA shortages, therefore deeming patient homes as a reimbursable telehealth, originating site. This revision allows patients who once had to travel to a clinic site to have a telehealth visit, to now access these services from the comforts of their own home. This shift aligns with HRS’ design - we typically partner with post-acute patient populations who receive care from their houses. In doing so, this solution reduces patients’ exposure to the virus while continuing to meet their healthcare needs.
On average, FQHC telehealth payments are $92 for CY 2020, which is based on the volume-weighted average amount for all telehealth services on the Medicare Physician Fee Schedule. For more information on billing and payments check out this article.
FQHCs and Remote Patient Monitoring
At this time Medicare does not reimburse FQHCs for remote patient monitoring (RPM) services while some state’s Medicaid and private insurers do. However, the growing driver of remote patient monitoring adoption amongst FQHCs is through grant opportunities. For example, several FQHCs received grant funding to expand virtual care models in support of the National Hypertension Control Initiative. In particular, this initiative helps FQHCS provide RPM services for the majority of their hypertensive patient population. While this funding definitely supports FQHCs’ adoption of remote patient monitoring, the long-term viability of these programs may be deemed as unsustainable given FQHC’s limited funding and resources.
However, by leveraging RPM services, FQHCs would achieve a substantial ROI that could offset the costs of RPM. There is evidence that remotely monitored patients will have decreased readmissions and ED utilization, which are key drivers of healthcare costs. For FQHCs that have risk arrangements with managed care organizations (MCOs), leveraging RPM would also result in higher reimbursement from the MCO by decreasing patient utilization, adding to overall cost-savings. RPM also plays a critical role in screening for COVID-19. Despite state and federal measures expanding telehealth coverage prompted by the pandemic, these freedoms will end with the emergency. However, our Director of Reimbursement, Gerald Buggs, states “once CMS sees the efficacy of telehealth services in reducing utilization, CMS may change their reimbursement guidelines permanently.” As the benefits of telehealth become more apparent, Health Recovery Solutions anticipates telehealth adoption to be both more permanent and pervasive amongst FQHCs.
