Based on the influx of research studies and position papers on social determinants of health flowing into my email box and Google Alerts, I can say we’re past the inflection point where SDoH is embraced by hospitals, professional societies, health plans and even a couple of pioneering pharma companies.
 PwC published a well-researched global-reaching report this week appropriately titled, Action required: The urgency of addressing social determinants of health. The “wheel of determinants” illustrates potential partners for collaborating in communities to address SDoH factors. The collaborators include governments, health care providers, payors, life science and pharma, tech and telecomms, policy and research, community-based organizations, and employers.
PwC published a well-researched global-reaching report this week appropriately titled, Action required: The urgency of addressing social determinants of health. The “wheel of determinants” illustrates potential partners for collaborating in communities to address SDoH factors. The collaborators include governments, health care providers, payors, life science and pharma, tech and telecomms, policy and research, community-based organizations, and employers.
I would add more granularly retail, education, and faith-based organizations. The latter may be classified as “community organizations,” but they can play an intimate, trusted role in many peoples’ health-and-wellness both spiritually and socially.
The report calls out “financial and biological metrics” which are really impactful to patients, particularly in the U.S., who are bearing more financial risks for paying for medical care. Concepts such as cost-per-health-condition and social return-on-investment are especially salient in this environment, which calculate positive externalities beyond a medical outcome and embody quality of life for the person, social connectedness, and community economic development aspects that can speak to “flourishing” beyond “survival.”
[Sidebar: this JAMA Viewpoint on Reimagining Health – Flourishing informs my view here – “the concept of flourishing has the potential to capture health more broadly than existing wellness measures for both patients and populations…could open a national conversation that reframes and reimagines traditional concepts of health”].
 JAMA featured research earlier this month showing that, while there is “swelling momentum for addressing social needs,” most physicians and hospitals are not screening across 5 key social needs associated with health outcomes (interpersonal violence, transportation, food security, housing stability and utility needs). The key barriers to screening were identified as lack of time available to spend with patients to discuss social factors, information and evidence on the SDoH, and money – that is, reimbursement to cover addressing social needs in the health care system.
JAMA featured research earlier this month showing that, while there is “swelling momentum for addressing social needs,” most physicians and hospitals are not screening across 5 key social needs associated with health outcomes (interpersonal violence, transportation, food security, housing stability and utility needs). The key barriers to screening were identified as lack of time available to spend with patients to discuss social factors, information and evidence on the SDoH, and money – that is, reimbursement to cover addressing social needs in the health care system.
Research published in Medical Care in June 2019 looked into clinician experiences and attitudes for screening SDoH in a large health system, and found the vast majority of clinicians supported efforts to incorporate social needs into clinical care — agreeing, too, that screening for social needs should become a standard part of care. However, lack of time, resources to channel people to social services, and lack of training about how to respond were indeed barriers to undertaking SDoH screening among providers.
To cap these stories, I had the honor of being a judge last week at the Robert Wood Johnson Foundation Social Determinants of Health Innovation Challenge competition to select an innovator incorporating social determinants of health into a technology solution, convened at the Health 2.0 Conference. There were dozens of entries vetted before the final three were chosen, which demo’d live at the session. My fellow judges, Adam Dakin, Managing Director of Healthtech with Dreamit Ventures and Pamela Garmon Johnson, National VP in the Health Equity Impact and Partnership program of the American Heart Association, and I wrestled with three great concepts. The final winner was the Social Impact AI Lab. The project brings together MercyFirst of New York City with Augmented Intelligence, a tech company that enables the human services agency network to scan and digest case social workers’ case notes using natural language processing AI. The team is developing the platform that can be scaled to other agencies beyond New York. This solution helps streamline Old School social workers’ notes by applying AI that parses the words in countless pages of notes and pulls out key social determinant factors — such as job loss, domestic violence, substance use, homelessness, and other challenges people face.
As I mindfully wrote in the title of this post — social determinants are just real life for Everyday People.
 Health Populi’s Hot Points: There’s been a tweet-storm of a debate spawned by an editorial in the Wall Street Journal published 12th September 2019, written by a former dean of the Medical School at the University of Pennsylvania, Dr. Stanley Goldfarb, titled “Take Two Aspirin and Call Me By My Pronouns.” The subtitle of the piece was, “At ‘woke’ medical schools, curricula are increasingly focused on social justice rather than treating illness.”
Health Populi’s Hot Points: There’s been a tweet-storm of a debate spawned by an editorial in the Wall Street Journal published 12th September 2019, written by a former dean of the Medical School at the University of Pennsylvania, Dr. Stanley Goldfarb, titled “Take Two Aspirin and Call Me By My Pronouns.” The subtitle of the piece was, “At ‘woke’ medical schools, curricula are increasingly focused on social justice rather than treating illness.”
Dr. Eric Topol launched a conversation in response to the op-ed which has a long thread you can review if you want to read the fine print of the debate. Suffice it to say there is a lot more discussion to be had on the roles of social science, social justice, health equity, and bias in academic and community medicine.
Over 150 graduates from Penn Medicine wrote this letter, published in Medscape, in response to the Wall Street Journal essay.
My own addition to the Twitter dialogue focused on this map image taken from my book, HealthConsuming, featured in the chapter, “ZIP Codes, Genetic Codes, Food and Health,” covering the impact of social determinants on all of our individual and communities’ health status.
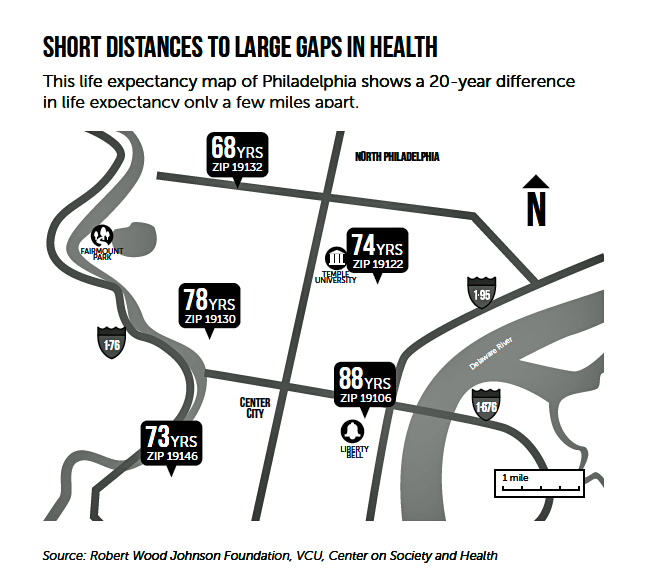 This image is a map illustrating the “short distances to large gaps in health” in Philadelphia, my home town. If you live by the Liberty Bell in ZIP code 19106 (look at the southeastern portion of the map), you can live to the ripe age of 88 years. If you reside northwest in ZIP code 19132, you may live on average 20 fewer years, dying at 68. This risk of mortality happens within a mere few miles’ difference in the City of Brotherly Love.
This image is a map illustrating the “short distances to large gaps in health” in Philadelphia, my home town. If you live by the Liberty Bell in ZIP code 19106 (look at the southeastern portion of the map), you can live to the ripe age of 88 years. If you reside northwest in ZIP code 19132, you may live on average 20 fewer years, dying at 68. This risk of mortality happens within a mere few miles’ difference in the City of Brotherly Love.
It’s ironic that Dean Goldfarb led a medical school in Philly. But we’d find similar mortality risks influenced by SDoH whether in New York City, Los Angeles, Miami, or Chicago.
Social determinants are all of our business, and patients/consumers/health citizens want to engage in health across all industry sectors.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.