U.S. employers are tightening their focus on mental and behavioral health, addressing workers’ chronic conditions, emphasizing women’s health, and allocating more resources to digital and telehealth investments, we learn from Optum’s Ten Years of Health and Well-Being at Work: Learning from our past and reimagining the future.
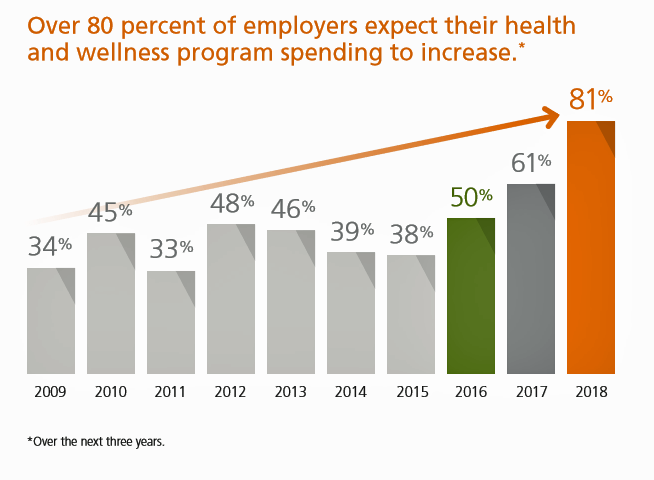
Four in five medium, large and jumbo companies expect their spending on health and wellness programs will increase over the next three years. That spending will have a strong focus on behavioral health services: 9 in 10 employers are concerned with the level of access workers have to mental health services. Companies will prioritize integrating behavioral health into medical care, implementing digital tools, growing provider networks, and implementing virtual visits — that is, tele-mental health (for more on this, please see my report written for the California HealthCare Foundation, The Online Couch: Mental Health Care on the Web). Of key import is the finding that 9 in 10 employers have plans to address mental health stigma in the next year.
What’s underlying employers’ commitment to address mental/behavioral health is that most companies believe that when these programs integrate with physical health services, employers achieve better health outcomes.
84% of employers are also concerned with substance use disorder, both for alcohol and opioids. The most prevalent actions employers plan to take will be to provide educational communications, alter benefit design to add in substance use programs, leverage EAP resources, and offer counseling.
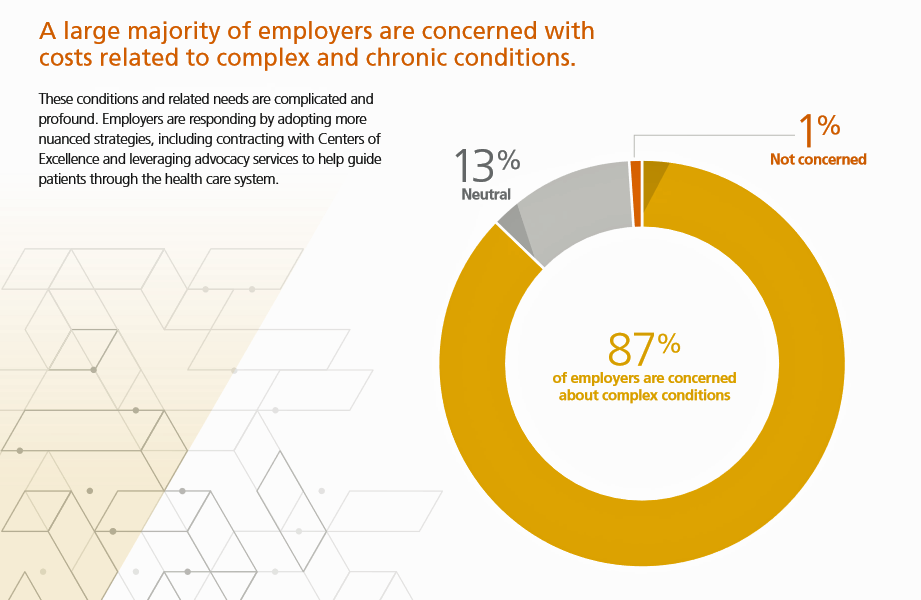 On the physical health side, employers are getting much more engaged with addressing chronic and complex conditions for 9 in 10 companies. Identifying and referring to Centers of Excellence is a strategy gaining traction among larger employers, 78% of which plan to use CoEx to focus on orthopedic surgery, heart care, transplants, and other high-cost health services. Four in five larger employers are also using health advocacy services for helping employees navigate the health system. Specific services employers have found successful include improving health outcomes, driving productivity at work, improving utilization of appropriate health systems (right service, right time, right patient), increasing employee satisfaction with health benefits, among other positive experiences.
On the physical health side, employers are getting much more engaged with addressing chronic and complex conditions for 9 in 10 companies. Identifying and referring to Centers of Excellence is a strategy gaining traction among larger employers, 78% of which plan to use CoEx to focus on orthopedic surgery, heart care, transplants, and other high-cost health services. Four in five larger employers are also using health advocacy services for helping employees navigate the health system. Specific services employers have found successful include improving health outcomes, driving productivity at work, improving utilization of appropriate health systems (right service, right time, right patient), increasing employee satisfaction with health benefits, among other positive experiences.
Employers are increasingly adopting digital health tech to nudge and drive sustained healthy behaviors. Most larger companies say their investments in these tactics are paying off and successful. The key digital tech’s and tactics employees have embraced and value include online competitions and challenges, social networks, activity tracking devices (such as Fitbit’s growing corporate health offering), health-related text messaging, health-related mobile apps, virtual support, integration of 3rd party apps, artificial intelligence, and virtual reality.
One of the new-new areas companies are targeting is women’s health: 82% of larger companies say it’s “very important” to offer a women’s health program. In addition to maternity (the top-offered benefit), most larger companies are also offering programs for neonatal health, first-year of life support, fertility solutions, midlife solutions (think: menopause management), and preconception health. The growth or programs like Babyscripts partnering with companies and health plans is an example of this trend.
For the current-year study, Optum surveyed 544 medium, large and jumbo employers in December 2018 and January 2019. The ten-year insights include data from 435 large and jumbo-sized companies (medium-sized companies excluded).
 Health Populi’s Hot Points: I reviewed and opined on the 2020 National Business Group on Health’s study into Large Employers Health Care Strategy and Plan Design here in Health Populi through my consumer-health lens. I gained additional insights into the NBGH survey through employers’ eyes in the analysis from SHRM, the Society for Human Resources Management [FYI, the Society’s tagline is, “Better Workforces, Better World].
Health Populi’s Hot Points: I reviewed and opined on the 2020 National Business Group on Health’s study into Large Employers Health Care Strategy and Plan Design here in Health Populi through my consumer-health lens. I gained additional insights into the NBGH survey through employers’ eyes in the analysis from SHRM, the Society for Human Resources Management [FYI, the Society’s tagline is, “Better Workforces, Better World].
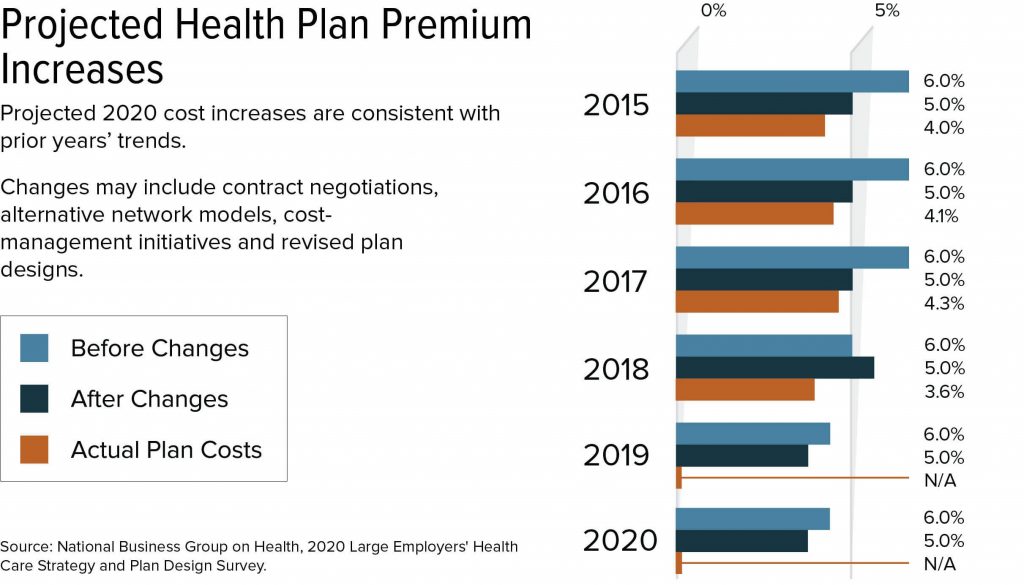
SHRM shows projected health plan premium increases in the last chart, shown from their website based on the NBGH data. SHRM represents employers, and so they assert that, “Large employers plan to use cost-management tactics to reduce projected health plan cost increases.”
While the Optum survey language and intent focused on employee health status improvement more than a pure cost approach, the NBGH survey, as SHRM knows, targets premiums and costs. Weaving the two together, it is clear that larger companies are embracing new tactics to help stem costs while also improving worker health — integrating both physical and mental/behavioral health status.
An important sidebar to consider: in this year’s Edelman Trust Barometer, the most trusted organizational category among global citizens was….the employer. This was a new finding for Edelman, as peoples’ trust in media, government, and even peers and each other has eroded over the past several years. That people are looking to the companies they work for support and a safe haven, we may be entering a new era of employee engagement. This will highly depend on the state of the national economy and labor force trends. But for now, the employer-as-trusted-health-touchpoint will be in our close-in forecast for the next 1-3 years.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.